Understanding Retinoschisis: Causes, Symptoms, Diagnosis, and Treatment
Retinoschisis is a condition that affects the eye’s retina, causing various visual disturbances. This comprehensive guide delves into the intricacies of retinoschisis, shedding light on its causes, symptoms, diagnosis, and treatment options. By understanding this condition better, you can take proactive steps towards maintaining your eye health.
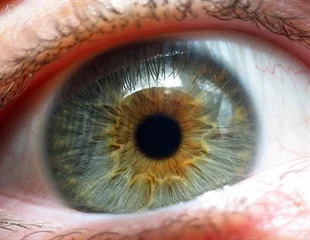
What is Retinoschisis?
Retinoschisis is a term used to describe the separation of the retina’s layers, leading to impaired vision. It’s essential to differentiate retinoschisis from other eye conditions for accurate diagnosis and treatment planning. The condition can be categorized into different types, each with distinct characteristics and impact on vision.
Causes and Risk Factors
Several factors contribute to the development of retinoschisis, with genetic predisposition and age-related changes playing a significant role. A family history of retinal conditions and certain medical conditions, such as myopia (nearsightedness), can elevate the risk. Understanding these causes and risk factors is crucial for early detection and management.
Types of Retinoschisis
Retinoschisis manifests in various forms, including juvenile and acquired retinoschisis. In juvenile retinoschisis, typically diagnosed in childhood, the retinal layers split, affecting central vision. Acquired retinoschisis, prevalent in adults, often presents with peripheral vision issues. Recognizing the types helps in identifying specific symptoms and planning appropriate treatments.
Symptoms and Signs
One of the key aspects of retinoschisis is its distinct set of symptoms. Blurred vision, particularly in the central or peripheral areas, is a common early sign. Peripheral vision loss can also occur, affecting your ability to see objects at the sides. This may lead to difficulty in navigating and recognizing faces. If you experience any of these symptoms, seeking professional medical attention promptly is essential for proper diagnosis and management.
Diagnosis and Detection
Accurate diagnosis of retinoschisis involves a comprehensive eye examination. Eye care professionals use advanced imaging techniques, including Optical Coherence Tomography (OCT), to visualize the retinal layers and identify any abnormalities. Early detection through regular eye check-ups can significantly impact the effectiveness of treatment strategies.
Treatment Options
Effective management of retinoschisis requires a tailored approach based on the severity and type of the condition. While some cases may require only observation and regular monitoring, others might benefit from surgical interventions. Vitrectomy, a surgical procedure to remove vitreous gel, can help reattach the retina’s layers and improve vision. Your eye care specialist will guide you in choosing the most suitable treatment plan for your situation.
Lifestyle Tips for Managing Retinoschisis
While medical interventions play a crucial role in managing retinoschisis, adopting a healthy lifestyle can complement your treatment plan. Incorporating foods rich in antioxidants, omega-3 fatty acids, and vitamins A, C, and E can support overall eye health. Additionally, regular exercise and avoiding smoking contribute positively to maintaining your vision.
Future Developments and Research
Ongoing research in the field of retinoschisis holds the promise of innovative treatment approaches. Scientists are exploring methods to stimulate retinal healing and regeneration, potentially revolutionizing how we manage this condition. Staying informed about advancements can empower individuals with retinoschisis to make informed decisions about their treatment journey.
Frequently Asked Questions (FAQs) About Retinoschisis
Q1: What is retinoschisis?
A1: Retinoschisis is a medical condition where the layers of the retina separate, leading to vision impairment.
Q2: What causes retinoschisis?
A2: Retinoschisis can be caused by genetic factors, age-related changes, and underlying medical conditions.
Q3: Are there different types of retinoschisis?
A3: Yes, retinoschisis can be categorized into types such as juvenile and acquired, each with distinct characteristics.
Q4: What are the symptoms of retinoschisis?
A4: Common symptoms include blurred vision, peripheral vision loss, and difficulty recognizing faces.
Q5: How is retinoschisis diagnosed?
A5: Diagnosis involves comprehensive eye exams and imaging tests like Optical Coherence Tomography (OCT).
Q6: Can retinoschisis lead to blindness?
A6: While severe cases can impact vision, early detection and proper management can help prevent blindness.
Q7: Is retinoschisis treatable?
A7: Yes, treatment options include observation, surgical procedures like vitrectomy, and lifestyle adjustments.
Q8: Are there ways to prevent retinoschisis?
A8: While prevention is challenging, maintaining overall eye health through a balanced lifestyle is beneficial.
Q9: How often should I get my eyes checked for retinoschisis?
A9: Regular eye exams are recommended, especially if you experience symptoms or have a family history of retinal issues.
Q10: What is the prognosis for individuals with retinoschisis?
A10: Prognosis varies based on factors like type and severity, but early intervention and proper care improve outcomes.
Conclusion
Retinoschisis is a complex eye condition that demands attention and proactive care. By understanding its causes, symptoms, and available treatment options, you can take charge of your eye health journey. Regular eye check-ups, early intervention, and embracing a healthy lifestyle are integral to maintaining optimal vision. Stay informed, stay vigilant, and prioritize your eyesight for a brighter future.




