Osteoarthritis vs Rheumatoid Arthritis: Understanding the Differences
When it comes to joint pain and discomfort, two conditions often come into play: osteoarthritis and rheumatoid arthritis. These conditions, although they share some similarities, have distinct characteristics that can significantly impact diagnosis and treatment. In this comprehensive guide, we’ll explore the differences between osteoarthritis and rheumatoid arthritis, shedding light on their symptoms, causes, and treatment options.
What Is Osteoarthritis?
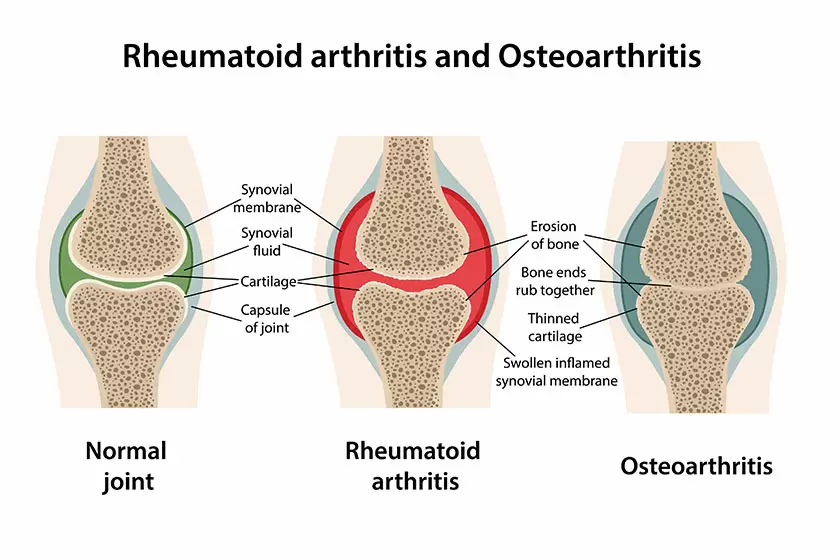
osteoarthritis vs. rheumatoid arthritis
Osteoarthritis Defined:
Osteoarthritis is a prevalent form of arthritis that primarily affects the joints.
It’s often associated with age-related wear and tear on joint cartilage.
Common Symptoms:
Joint stiffness, particularly after periods of inactivity.
Pain, which worsens with joint use.
Natural language processing tip: “Osteoarthritis pain typically starts as a dull ache and progresses over time.”
Risk Factors:
Age, as it’s more common in older individuals.
Joint injuries or overuse.
Family history and genetics.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis Defined:
Rheumatoid arthritis is an autoimmune disorder characterized by joint inflammation.
The immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints.
Common Symptoms:
Joint swelling and tenderness.
Morning stiffness, lasting for hours.
Risk Factors:
Gender, as it’s more common in women.
Family history and genetics.
Smoking and environmental factors.
Distinguishing Symptoms
Recognizing Osteoarthritis Symptoms:
Osteoarthritis primarily affects weight-bearing joints like the knees, hips, and spine.
Joint pain typically worsens with activity and improves with rest.
Natural language processing tip: “Osteoarthritis pain can be described as aching and may be accompanied by a cracking or grating sensation in the affected joint.”
Recognizing Rheumatoid Arthritis Symptoms:
Rheumatoid arthritis can affect any joint, including small joints like those in the hands and feet.
Joint pain tends to be symmetrical, meaning it affects both sides of the body.
Causes and Risk Factors
Contributing Factors to Osteoarthritis:
Age-related wear and tear on joint cartilage.
Joint injuries from sports or accidents.
Family history and genetics.
Factors Underlying Rheumatoid Arthritis:
Autoimmune response causing joint inflammation.
Genetic predisposition.
Environmental triggers that may include infections.
Diagnosis
Osteoarthritis Diagnosis:
Based on symptoms, physical examination, and imaging (X-rays, MRI).
This may involve ruling out other conditions.
Rheumatoid Arthritis Diagnosis:
Blood tests, including rheumatoid factor and anti-CCP antibodies.
Imaging studies like X-rays and ultrasounds.
Synovial fluid analysis.
Treatment Options
Managing Osteoarthritis:
Lifestyle modifications, including weight management and exercise.
Pain-relieving medications.
Physical therapy and assistive devices.
Treating Rheumatoid Arthritis:
Disease-modifying antirheumatic drugs (DMARDs).
Biologics targeting the immune system.
Pain management and physical therapy.
Living with Arthritis
Coping Strategies for Osteoarthritis:
Incorporating joint-friendly exercises into daily routines.
Maintaining a healthy diet for weight control.
Seeking support from physical therapists or support groups.
Coping with Rheumatoid Arthritis:
Balancing rest and exercise to manage symptoms.
Utilizing assistive devices to ease daily tasks.
Emotional support from loved ones and counseling.
Prevention and Outlook
Preventing Osteoarthritis:
Emphasize joint-friendly activities and exercises.
Maintain a healthy weight to reduce joint stress.
Minimize the risk of joint injuries.
Preventing Rheumatoid Arthritis:
No known prevention methods, but early diagnosis and treatment are crucial.
Consulting a Specialist
Osteoarthritis Specialist:
Orthopedic specialists can provide tailored treatment plans.
Physical therapists for rehabilitation.
Rheumatoid Arthritis Specialist:
Rheumatologists are experts in autoimmune joint disorders.
Collaborative care with physical therapists.
FAQs:
1. What is the primary difference between osteoarthritis and rheumatoid arthritis?
Answer: Osteoarthritis is primarily due to wear and tear on joint cartilage, while rheumatoid arthritis is an autoimmune disorder causing joint inflammation.
2. Can age be a risk factor for both conditions?
Answer: Yes, age is a significant risk factor for osteoarthritis, especially in older individuals. Rheumatoid arthritis, on the other hand, can affect people of all ages.
3. How do I recognize early symptoms of arthritis?
Answer: Common early signs include joint stiffness, pain, and swelling. In rheumatoid arthritis, morning stiffness that lasts for hours is a notable symptom.
4. Are there any preventative measures for arthritis?
Answer: While you can’t always prevent arthritis, maintaining a healthy weight, regular exercise, and avoiding joint injuries can reduce the risk.
5. What role do genetics play in these conditions?
Answer: Genetics can increase susceptibility to both osteoarthritis and rheumatoid arthritis. A family history of arthritis can raise the risk.
6. Can arthritis affect daily life and mobility?
Answer: Yes, arthritis can impact mobility and daily activities. Effective management and lifestyle adjustments can help maintain quality of life.
7. Are there specific medications for arthritis treatment?
Answer: Yes, medication options vary for each type of arthritis. For rheumatoid arthritis, disease-modifying antirheumatic drugs (DMARDs) are commonly used.
8. Is there a cure for arthritis?
Answer: Currently, there is no cure for arthritis, but early intervention and proper management can significantly reduce symptoms and improve quality of life.
9. Should I consult a specialist for arthritis diagnosis and treatment?
Answer: Consulting a specialist, such as an orthopedic doctor for osteoarthritis or a rheumatologist for rheumatoid arthritis, ensures accurate diagnosis and tailored treatment plans.
10. Can arthritis be hereditary?
Answer: Yes, a family history of arthritis can increase the likelihood of developing the condition. Genetic factors play a role in arthritis susceptibility.
Conclusion
Summarize the distinct characteristics of osteoarthritis and rheumatoid arthritis. Stress the importance of early diagnosis and appropriate treatment. Advise readers to consult healthcare experts for personalized care.




