Understanding PNH: Paroxysmal Nocturnal Hemoglobinuria
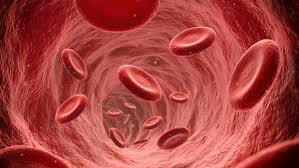
Paroxysmal Nocturnal Hemoglobinuria (PNH) is a rare and complex blood disorder characterized by the abnormal breakdown of red blood cells. This condition is caused by a mutation in the PIGA gene, leading to the deficiency of certain proteins on the surface of blood cells. As a result, affected individuals experience a range of symptoms and challenges that impact their quality of life.
Causes and Genetic Basis
PNH is primarily caused by a genetic mutation in the PIGA gene. This mutation affects the production of glycosylphosphatidylinositol (GPI) anchors, which are essential for attaching specific proteins to the surface of blood cells. Without these proteins, red blood cells become more susceptible to destruction by the immune system, leading to the characteristic symptoms of PNH.
The genetic nature of PNH means that it can be inherited or occur spontaneously due to a new mutation. Genetic testing and counseling are essential for individuals with a family history of PNH or those who are considering having children.
Symptoms and Clinical Presentation
PNH can manifest with a wide range of symptoms, and their severity can vary among individuals. Common symptoms include:
Hemolytic Anemia:
The rapid destruction of red blood cells results in anemia, leading to fatigue, weakness, and shortness of breath.
Hemoglobinuria:
Dark-colored urine due to the presence of hemoglobin released from damaged red blood cells.
Thrombosis:
Blood clots can form in veins, leading to serious complications such as stroke or heart attack.
Bone Marrow Failure:
PNH can lead to bone marrow failure, affecting the production of other blood cells such as platelets and white blood cells.
It’s important to note that PNH symptoms can worsen over time and lead to serious health risks. Early diagnosis and appropriate management are crucial for improving outcomes and quality of life.
Diagnosis and Medical Evaluation
Diagnosing PNH requires a comprehensive medical evaluation, including:
Blood Tests:
Tests for levels of hemoglobin, red blood cells, white blood cells, and platelets can help identify abnormalities.
Flow Cytometry:
This specialized test helps detect the absence or reduced expression of specific proteins on blood cells.
Bone Marrow Biopsy:
A sample of bone marrow is examined to assess its health and functionality.
Genetic Testing:
Genetic analysis can confirm the presence of the PIGA gene mutation.
Treatment Options for PNH: Managing the Condition
Managing PNH involves a multidisciplinary approach that aims to alleviate symptoms, prevent complications, and improve the overall quality of life for individuals affected by the condition.
Targeted Therapies and Monoclonal Antibodies
Recent advancements in the understanding of PNH have led to the development of targeted therapies and monoclonal antibodies that specifically address the underlying cause of the condition. These therapies work by inhibiting the complement system, which is responsible for the destruction of red blood cells. By blocking this process, targeted therapies can reduce hemolysis and improve symptoms.
Blood Transfusions and Supportive Care
For individuals with severe anemia, regular blood transfusions may be necessary to maintain adequate hemoglobin levels. Additionally, supportive care measures such as folic acid supplementation and iron chelation therapy can help manage symptoms and complications.
Hematopoietic Stem Cell Transplantation
In some cases, hematopoietic stem cell transplantation (HSCT) may be considered for individuals with severe PNH. HSCT involves replacing the faulty bone marrow with healthy donor cells to restore normal blood cell production. However, HSCT carries significant risks and is typically reserved for cases where other treatment options have been exhausted.
Managing PNH-Related Complications
Thrombosis Prevention
Given the increased risk of blood clots in individuals with PNH, preventive measures are crucial. Anticoagulant medications, lifestyle modifications, and close medical monitoring can help reduce the risk of thrombosis.
Bone Marrow Transplantation
For individuals with bone marrow failure, bone marrow or stem cell transplantation may be considered. This procedure aims to replace diseased bone marrow with healthy donor cells, allowing for the production of healthy blood cells.
Long-Term Care and Monitoring
Regular follow-up appointments with healthcare professionals specializing in hematology are essential for individuals with PNH. Ongoing monitoring helps track disease progression, adjust treatment plans, and address any emerging complications.
Lifestyle Considerations and Support
Maintaining Overall Health
Adopting a healthy lifestyle that includes a balanced diet, regular exercise, and adequate sleep can complement medical treatments and improve overall well-being for individuals with PNH.
Patient Support and Advocacy
Support groups and advocacy organizations provide valuable resources, information, and a sense of community for individuals living with PNH. Connecting with others who share similar experiences can offer emotional support and practical advice.
Research and Future Directions
Advancements in research continue to shed light on PNH, leading to improved understanding and potential breakthroughs in treatment. Researchers are exploring innovative therapies that target specific aspects of the condition’s molecular basis.
Clinical Trials and Emerging Therapies
Participating in clinical trials can provide individuals with PNH access to experimental treatments that have the potential to revolutionize care. These trials are essential for evaluating the safety and efficacy of new therapies.
Collaboration and Medical Progress
Collaboration between healthcare professionals, researchers, and patients is driving medical progress in the field of PNH. This collaboration is instrumental in developing comprehensive treatment plans that address individual needs.
Frequently Asked Questions About PNH
1. What is PNH?
PNH stands for Paroxysmal Nocturnal Hemoglobinuria, a rare blood disorder characterized by the abnormal breakdown of red blood cells.
2. What causes PNH?
PNH is primarily caused by a genetic mutation in the PIGA gene, leading to the deficiency of specific proteins on blood cells.
3. What are the common symptoms of PNH?
Common symptoms of PNH include hemolytic anemia, dark-colored urine, thrombosis, and bone marrow failure.
4. How is PNH diagnosed?
PNH is diagnosed through blood tests, flow cytometry, bone marrow biopsy, and genetic testing.
5. Is PNH hereditary?
Yes, PNH can be inherited or occur spontaneously due to a new mutation.
6. What are the available treatments for PNH?
Treatments for PNH include targeted therapies, monoclonal antibodies, blood transfusions, and hematopoietic stem cell transplantation.
7. Are there preventive measures for thrombosis in PNH?
Yes, anticoagulant medications, lifestyle changes, and medical monitoring can help reduce the risk of blood clots.
8. What is hematopoietic stem cell transplantation?
Hematopoietic stem cell transplantation involves replacing faulty bone marrow with healthy donor cells to restore normal blood cell production.
9. How can individuals with PNH maintain their overall health?
A balanced diet, regular exercise, and sufficient sleep contribute to overall well-being for individuals with PNH.
10. What are the latest developments in PNH research?
Ongoing research and clinical trials explore emerging therapies and advancements in the treatment of PNH.
Conclusion
Paroxysmal Nocturnal Hemoglobinuria (PNH) is a complex condition that requires a personalized and multidisciplinary approach to management. By understanding the genetic basis, symptoms, and treatment options, individuals with PNH can work closely with healthcare professionals to optimize their quality of life.




