Demystifying the Maculopapular Rash Causes, Symptoms, and Treatment
A maculopapular rash is a common dermatological condition characterized by its distinctive appearance and potential association with various underlying causes. In this comprehensive guide, we will demystify the maculopapular rash, exploring its defining features and shedding light on the underlying triggers.
Understanding Maculopapular Rashes
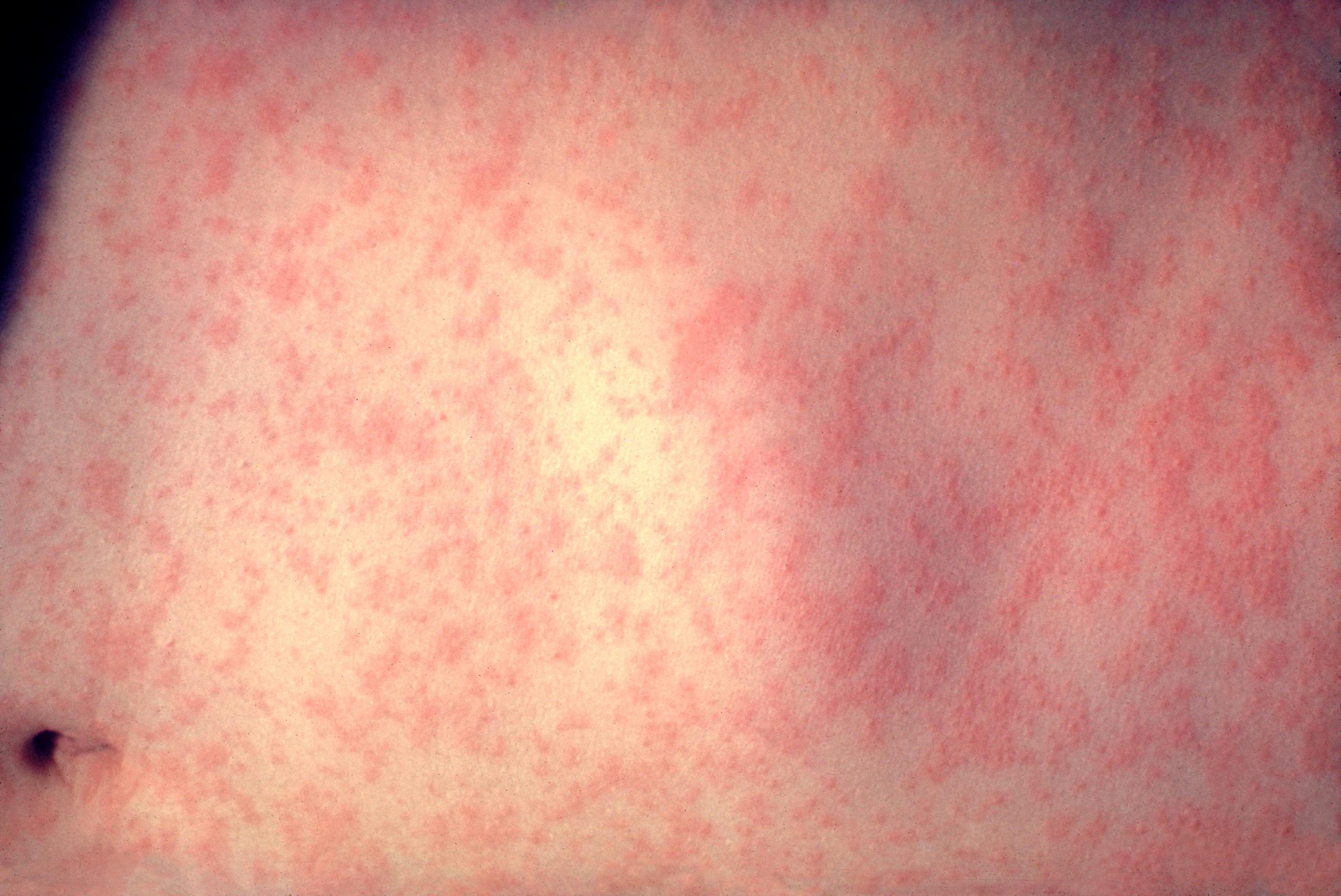
Understanding the characteristics of a maculopapular rash is the first step in recognizing and addressing this skin condition. A maculopapular rash is characterized by the presence of both macules and papules on the skin’s surface.
Macules:
These are flat, discolored spots on the skin that may vary in color and size. They can be red, brown, or even slightly pinkish.
Papules:
Papules are small, raised bumps on the skin. They often accompany macules in a maculopapular rash.
The combined presence of these two elements gives the rash its name—maculopapular. These rashes can appear anywhere on the body and are known for their varied appearance.
Common Causes and Triggers
Maculopapular rashes can result from a wide range of factors. While they may share a common appearance, their underlying causes can vary significantly. Here are some common causes and triggers:
Infections:
Viral and bacterial infections, such as measles, rubella, and scarlet fever, can lead to maculopapular rashes. These rashes often accompany other symptoms of the infection.
Drug Reactions:
Certain medications can trigger maculopapular rashes as adverse reactions. These rashes can range from mild to severe and may require discontinuation of the offending medication.
Allergies:
Allergic reactions to substances like foods, insect bites, or latex can result in maculopapular rashes. Identifying and avoiding the allergen is key to preventing recurrence.
Symptoms and Clinical Presentation
Recognizing the symptoms and clinical presentation of a maculopapular rash is crucial for early identification and potential diagnosis. Common characteristics of these rashes include:
Reddish or brownish spots (macules)
Small raised bumps (papules)
Itching or discomfort
Distribution across the body, often starting on the trunk and spreading
Variable sizes and shapes of macules and papules
It’s important to note that while these are common features, maculopapular rashes can present differently based on their underlying cause. Therefore, a thorough evaluation by a healthcare professional is essential.
Diagnosis and Medical Evaluation
Diagnosing a maculopapular rash involves a combination of clinical assessment, medical history, and, in some cases, diagnostic tests. Here’s an overview of the diagnostic process:
Medical History:
Your healthcare provider will inquire about recent illnesses, medication use, allergies, and exposure to potential triggers.
Physical Examination:
A visual examination of the rash’s appearance and distribution is a critical step in diagnosis.
Diagnostic Tests:
In some cases, blood tests or skin biopsies may be recommended to identify the underlying cause, especially if infections are suspected.
Treatment and Management
Managing a maculopapular rash depends on its underlying cause. Here are some general guidelines:
Infections:
If an infection is the culprit, treatment will target the specific pathogen responsible. Antiviral or antibacterial medications may be prescribed.
Drug Reactions:
Discontinuing the offending medication is typically the first step. Consult your healthcare provider for guidance on alternative medications if necessary.
Allergies:
Identifying and avoiding the allergen is key. Antihistamines or topical corticosteroids may provide relief from itching and discomfort.
Prevention and Outlook
Preventing a maculopapular rash depends on its underlying causes. However, some general preventive measures can be considered:
Infections:
Practicing good hygiene, receiving vaccinations when appropriate, and avoiding close contact with infected individuals can help reduce the risk of infection-related rashes.
Drug Reactions:
Communicate any known allergies or previous adverse reactions to medications with healthcare providers to prevent drug-related rashes.
Allergies:
Identify and avoid allergens when possible. If you have known allergies, carry appropriate medications (e.g., epinephrine for severe allergic reactions) as a precaution.
When to Seek Medical Attention
While some maculopapular rashes may resolve on their own, others can be indicators of more serious underlying conditions. It’s important to know when to seek immediate medical attention:
Severe Symptoms:
If the rash is accompanied by severe symptoms like difficulty breathing, swelling of the face or throat, or a high fever, seek medical help immediately.
Worsening Condition:
If the rash worsens or spreads rapidly, it may be a sign of a serious infection or allergic reaction.
Persistent Rash:
If the rash persists for an extended period without improvement, consult a healthcare provider for evaluation.
Complications and Associated Conditions
Maculopapular rashes themselves may not always lead to complications, but they can be indicative of underlying conditions that require attention. Complications and associated conditions may include:
Secondary Infections:
Scratching the rash can introduce bacteria and lead to secondary skin infections.
Allergic Reactions:
In some cases, maculopapular rashes due to allergies can escalate into severe allergic reactions.
Underlying Diseases:
Certain infections or medical conditions that cause maculopapular rashes may require specific treatments.
Frequently Asked Questions (FAQs) About Maculopapular Rashes
1. What is a maculopapular rash?
A maculopapular rash is a skin condition characterized by flat, discolored spots (macules) and small, raised bumps (papules) on the skin’s surface. It’s a common rash with various underlying causes.
2. What causes maculopapular rashes?
Maculopapular rashes can be caused by infections (viral or bacterial), drug reactions, allergies, or underlying medical conditions. Identifying the cause is essential for appropriate treatment.
3. Are maculopapular rashes contagious?
The rash itself is not contagious, but if it results from an infectious disease like measles or chickenpox, the underlying illness may be contagious. Proper precautions and isolation are necessary.
4. What do maculopapular rashes look like?
Maculopapular rashes typically consist of red or brownish flat spots (macules) interspersed with small raised bumps (papules). The rash may vary in size, shape, and distribution.
5. Can maculopapular rashes cause itching?
Yes, many maculopapular rashes can cause itching or discomfort. The level of itching can vary depending on the underlying cause and the individual’s sensitivity.
6. How are maculopapular rashes diagnosed?
Diagnosis involves a medical history review, physical examination, and sometimes diagnostic tests like blood work or skin biopsies. Identifying the underlying cause is crucial.
7. What is the treatment for maculopapular rashes?
Treatment depends on the cause. For infections, antiviral or antibacterial medications may be prescribed. For drug reactions, discontinuing the medication is often necessary. Allergies may be managed with antihistamines or corticosteroids.
8. Can maculopapular rashes go away on their own?
Some maculopapular rashes may resolve on their own, especially if they result from a mild viral infection. However, others may require specific treatment to improve.
9. Are maculopapular rashes dangerous?
Maculopapular rashes themselves are usually not dangerous. However, they can be indicators of underlying conditions that require attention. Seeking medical evaluation is important.
10. How can I prevent maculopapular rashes?
Preventive measures depend on the cause. Practicing good hygiene, receiving vaccinations, and avoiding known allergens or irritants can help prevent some types of maculopapular rashes.
Conclusion:
In conclusion, understanding maculopapular rashes, their symptoms, and potential causes is essential for both individuals experiencing them and healthcare professionals. While some rashes may resolve with time and self-care, others may require specific treatments. Remember that this guide serves as an informative resource, but individual cases should be evaluated by healthcare providers to determine the precise diagnosis and appropriate management.




