Differences Between Rheumatoid Arthritis vs Osteoarthritis: Know the Contrast
Arthritis is a term that encompasses various joint conditions, each with its unique characteristics and impacts. In this comprehensive guide, we’ll shed light on the distinctions between two prevalent forms of arthritis: Rheumatoid Arthritis (RA) and Osteoarthritis (OA).
Understanding Rheumatoid Arthritis (RA)
To comprehend the differences between RA and OA, it’s crucial to first understand Rheumatoid Arthritis.
What Is Rheumatoid Arthritis (RA)?
Rheumatoid Arthritis (RA) is an autoimmune disease that affects approximately 1.3 million Americans. It occurs when the immune system mistakenly attacks healthy joint tissues, leading to inflammation, pain, and joint damage.
The Autoimmune Nature of RA
RA is characterized by its autoimmune nature, where the immune system’s malfunction triggers inflammation in the synovium—the lining of the membranes that surround joints. This inflammation can ultimately lead to joint erosion and deformities if left untreated.
The Importance of Early Diagnosis
One of the key factors in managing RA effectively is early diagnosis. Recognizing the symptoms and seeking prompt medical attention is critical to slowing the progression of the disease and preserving joint function.
Understanding Osteoarthritis (OA)
Now that we have a grasp of Rheumatoid Arthritis (RA), let’s turn our attention to Osteoarthritis.
What Is Osteoarthritis (OA)?
Osteoarthritis (OA) is the most common type of arthritis, affecting millions of people worldwide. Unlike RA, OA is not an autoimmune disease. Instead, it’s often referred to as a degenerative joint disease.
The Wear-and-Tear Aspect of OA
OA develops due to the wear and tear of joint cartilage over time. As cartilage—the protective cushion between bones—gradually breaks down, joints may become painful, stiff, and less flexible.
Common Risk Factors for OA
Several factors increase the risk of developing OA, including advancing age, joint injuries, and obesity. It typically affects weight-bearing joints such as the knees, hips, and spine.
Key Differences Between RA and OA
Now that we’ve established the basics of RA and OA, let’s delve into the fundamental differences between these two prevalent forms of arthritis.
Autoimmune vs. Degenerative
The most significant distinction lies in their underlying mechanisms. RA is an autoimmune disease, where the immune system mistakenly attacks joints. In contrast, OA is degenerative, primarily resulting from the natural aging process and joint wear and tear.
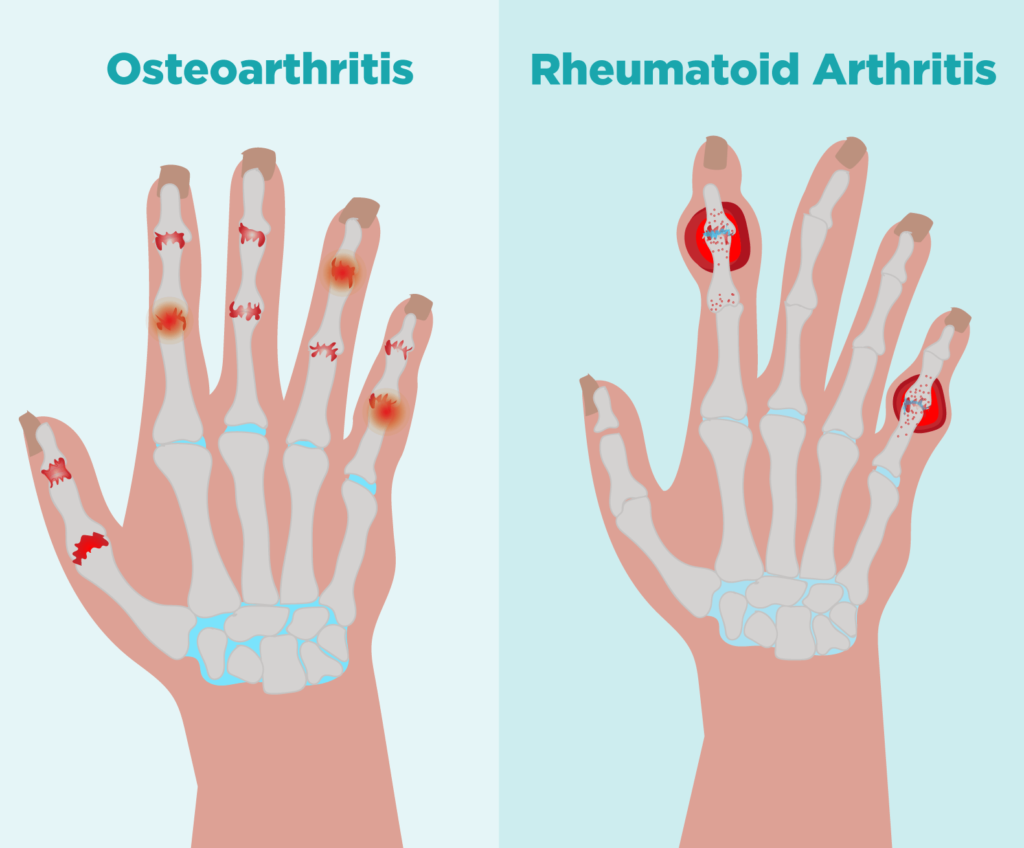
Joint Symptoms
RA often presents with symptoms in multiple joints simultaneously, including joint pain, stiffness, and swelling. In OA, symptoms typically affect a single joint or a few joints and include localized pain, limited range of motion, and joint enlargement.
Systemic vs. Localized
RA is systemic, meaning it can affect various parts of the body beyond joints, leading to fatigue, fever, and even organ involvement. OA is primarily localized to the affected joint and doesn’t have systemic effects.
Treatment Approaches
Treatment approaches differ significantly. RA management involves medications to suppress the immune response (DMARDs) and lifestyle adjustments. OA management focuses on pain relief, joint protection, and lifestyle modifications.
Symptoms of Rheumatoid Arthritis (RA)
Understanding the symptoms of Rheumatoid Arthritis (RA) is essential for early detection and effective management.
Common Symptoms of RA
RA often manifests with several hallmark symptoms:
Joint Pain:
Persistent joint pain, typically affecting multiple joints.
Joint Stiffness:
Stiffness, especially in the morning or after periods of inactivity.
Joint Swelling:
Swelling and warmth around affected joints.
Fatigue:
Overwhelming fatigue can significantly impact daily life.
Fever:
Occasional low-grade fevers may accompany RA flares.
Weight Loss:
Unintended weight loss can occur as a result of the disease’s systemic effects.
The Role of Inflammation
In RA, inflammation plays a central role in causing these symptoms. The immune system’s attack on joint tissues leads to redness, swelling, and pain.
Symmetrical Joint Involvement
One hallmark of RA is symmetrical joint involvement. For example, if the joints of the left wrist are affected, the right wrist is likely to be affected as well.
Symptoms of Osteoarthritis (OA)
Osteoarthritis (OA) presents with its distinct set of symptoms, primarily related to the affected joints.
Joint Pain and Stiffness
The hallmark symptom of OA is joint pain, often described as a deep ache. Stiffness may also occur, usually after periods of rest or inactivity.
Limited Range of Motion
OA can restrict joint movement, leading to a reduced range of motion. This can affect everyday activities like walking, climbing stairs, or bending.
Joint Enlargement
As OA progresses, joint enlargement or the formation of bony outgrowths called bone spurs can occur, causing joint deformities.
Crepitus
Some individuals with OA experience a crackling or grating sensation within the affected joint. This sensation, known as crepitus, is due to the roughened joint surfaces.
Symptoms Worsening with Activity
Unlike RA, OA symptoms often worsen with joint activity or weight-bearing. Overuse of the affected joint can lead to increased pain and discomfort.
Causes and Risk Factors
Understanding the causes and risk factors associated with Rheumatoid Arthritis (RA) and Osteoarthritis (OA) is essential to grasp why these conditions develop.
Causes of Rheumatoid Arthritis (RA)
Autoimmune Response:
RA is primarily caused by an autoimmune response. The exact trigger is unknown, but it’s believed to involve a combination of genetic and environmental factors.
Genetic Predisposition:
Certain genetic markers may increase susceptibility to RA.
Environmental Factors: Factors such as smoking and exposure to certain infections may contribute to RA development.
Risk Factors for Osteoarthritis (OA)
Age:
The risk of OA increases with advancing age.
Joint Injuries:
Prior joint injuries or trauma can predispose individuals to OA in those joints.
Obesity:
Excess body weight places additional stress on weight-bearing joints, such as the knees and hips, increasing the risk of OA.
Gender:
OA is more common in women, especially after menopause.
Joint Overuse:
Repetitive joint use in certain occupations or activities may contribute to OA development.
Diagnosis and Testing
Accurate diagnosis is vital for effective management of both Rheumatoid Arthritis (RA) and Osteoarthritis (OA).
Diagnosing Rheumatoid Arthritis (RA)
Clinical Evaluation:
Healthcare providers conduct a comprehensive clinical evaluation, assessing joint symptoms, medical history, and physical examination.
Blood Tests:
Blood tests, such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies, help confirm the presence of RA.
Imaging Studies:
Imaging techniques like X-rays and magnetic resonance imaging (MRI) help assess joint damage.
Diagnosing Osteoarthritis (OA)
Physical Examination:
OA diagnosis often begins with a physical examination, where joint pain, stiffness, and range of motion are evaluated.
Imaging Tests:
X-rays are commonly used to visualize joint changes associated with OA, including cartilage loss and bone spurs.
Joint Fluid Analysis:
In some cases, joint fluid analysis may be performed to rule out other conditions.
Treatment and Management
Managing Rheumatoid Arthritis (RA) and Osteoarthritis (OA) involves a combination of medical interventions and lifestyle adjustments.
Treating Rheumatoid Arthritis (RA)
Disease-Modifying Antirheumatic Drugs (DMARDs):
DMARDs are a cornerstone of RA treatment, as they help suppress the immune system’s response, reducing inflammation and joint damage.
Biologic Response Modifiers:
In some cases, biologics are prescribed to target specific immune system proteins involved in RA.
Pain Relief Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) and analgesics can help manage pain and inflammation.
Physical Therapy:
Physical therapy exercises improve joint function and reduce stiffness.
Lifestyle Modifications:
Lifestyle changes like managing stress, maintaining a healthy weight, and getting regular exercise can complement medical treatment.
Managing Osteoarthritis (OA)
Pain Management:
Pain relief is a primary goal in OA management. This may involve over-the-counter pain relievers or prescription medications.
Physical Therapy:
Physical therapists can guide individuals through exercises that help improve joint function and reduce pain.
Joint Protection:
Learning how to protect joints during daily activities can prevent OA symptoms from worsening.
Assistive Devices:
Devices like braces or shoe inserts can alleviate joint stress.
Weight Management:
Maintaining a healthy weight can reduce the strain on weight-bearing joints affected by OA.
Living with RA and OA
Living with Rheumatoid Arthritis (RA) or Osteoarthritis (OA) involves adapting to these conditions and making choices that promote well-being.
Pain Management Strategies
Explore various pain management strategies, including heat and cold therapy, to alleviate discomfort.
Consider acupuncture or mindfulness techniques to manage chronic pain.
Joint-Friendly Exercise
Engage in joint-friendly exercises such as swimming or low-impact aerobics to maintain joint mobility and reduce stiffness.
Assistive Devices
Embrace assistive devices like canes or ergonomic tools to make daily tasks easier on your joints.
Dietary Considerations
Adopt an anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids to help manage inflammation.
Emotional Well-being
Address the emotional aspects of living with chronic pain by seeking support from therapists or support groups.
Support and Resources
Navigating Rheumatoid Arthritis (RA) or Osteoarthritis (OA) can be challenging, but there are valuable resources and support available.
Support Groups
Joining local or online support groups connects you with individuals who understand your journey and can offer guidance and emotional support.
Healthcare Providers
Building a strong partnership with healthcare providers, including rheumatologists or orthopedic specialists, is essential for effective management.
Stay Informed
Stay informed about the latest developments in RA and OA research. Knowledge empowers you to make informed decisions about your health.
Medication Management
Understand your prescribed medications, their potential side effects, and the importance of adherence to your treatment plan.
Ongoing Research and Hope
Both Rheumatoid Arthritis (RA) and Osteoarthritis (OA) are subjects of ongoing research, offering hope for improved treatments and outcomes.
Advancements in Treatment
Stay updated on advancements in RA and OA treatment options, as new therapies continue to emerge.
Lifestyle Research
Research on lifestyle modifications and dietary choices may reveal additional ways to manage symptoms and improve joint health.
Participate in Research
Consider participating in clinical trials if you meet the criteria. Your involvement can contribute to future breakthroughs in arthritis treatment.
FAQs to Rheumatoid Arthritis (RA) and Osteoarthritis (OA)
Q: What is the primary difference between Rheumatoid Arthritis (RA) and Osteoarthritis (OA)?
A: RA is an autoimmune disease where the immune system attacks joints, while OA is a degenerative joint disease primarily caused by wear and tear.
Q: Can both RA and OA affect multiple joints?
A: RA often affects multiple joints simultaneously, while OA typically affects a single joint or a few joints.
Q: What are the systemic symptoms of Rheumatoid Arthritis (RA)?
A: RA can cause systemic symptoms such as fatigue, fever, and even organ involvement, unlike Osteoarthritis (OA).
Q: Is joint enlargement a common symptom of Osteoarthritis (OA)?
A: Yes, as OA progresses, joint enlargement and the formation of bone spurs can occur.
Q: Are there any genetic factors that increase the risk of Rheumatoid Arthritis (RA)?
A: Certain genetic markers may increase susceptibility to RA.
Q: Can joint injuries contribute to the development of Osteoarthritis (OA)?
A: Yes, prior joint injuries or trauma can predispose individuals to OA in those joints.
Q: What are the primary medications used to treat Rheumatoid Arthritis (RA)?
A: Disease-modifying antirheumatic Drugs (DMARDs) and biologics are commonly used to manage RA.
Q: How can pain be managed in Osteoarthritis (OA)?
A: Pain in OA can be managed through pain relief medications and physical therapy exercises.
Q: Are there any lifestyle modifications that can help in managing both RA and OA?
A: Yes, lifestyle changes like stress management, maintaining a healthy weight, and regular exercise can complement treatment.
Q: Are there support groups available for individuals with RA and OA?
A: Yes, there are local and online support groups that connect individuals affected by these conditions, offering guidance and emotional support.
Conclusion
In conclusion, understanding the differences between Rheumatoid Arthritis (RA) and Osteoarthritis (OA) is essential for individuals affected by these conditions. Early diagnosis, effective management, and a supportive network of resources can significantly enhance the quality of life for those living with RA or OA.




