Understanding Duodenal Cancer: Causes, Symptoms, and Treatment
Duodenal cancer is a rare yet significant form of cancer that originates in the duodenum, the first part of the small intestine. While it may be less common than other types of cancer, its impact on health cannot be underestimated. This comprehensive guide aims to provide valuable insights into duodenal cancer, including its causes, symptoms, and available treatment options. By understanding the nuances of this condition, individuals can make informed decisions about their health and well-being.
What is Duodenal Cancer?
Duodenal cancer refers to the malignant growth of cells within the duodenum, the initial segment of the small intestine. This form of cancer is categorized as a subtype of gastrointestinal cancer and primarily affects the lining of the duodenum. While it accounts for a small percentage of all cancer cases, its location and potential complications require careful attention.
Duodenal cancer can manifest in different forms, including adenocarcinomas and neuroendocrine tumors, each with unique characteristics and treatment approaches.
Causes and Risk Factors:
The exact cause of duodenal cancer is not always clear, but certain risk factors have been identified. These include genetic predisposition, inherited conditions like familial adenomatous polyposis (FAP), and environmental factors such as diet and smoking. Individuals with a family history of gastrointestinal cancers or those with inflammatory bowel diseases may face an elevated risk.
Importantly, a high-fat diet, smoking, and chronic inflammation can contribute to the development of duodenal cancer. Understanding these risk factors empowers individuals to make lifestyle changes that may reduce their vulnerability.
Symptoms and Early Detection:
Duodenal cancer’s early symptoms can be subtle and easily mistaken for other gastrointestinal issues. Common signs include abdominal discomfort, unexplained weight loss, nausea, vomiting, and changes in bowel habits. Due to the non-specific nature of these symptoms, individuals often delay seeking medical attention, underscoring the importance of awareness.
Early detection is key to successful treatment. Individuals experiencing persistent symptoms or having risk factors should promptly consult a healthcare professional for proper evaluation and diagnosis.
Diagnosing Duodenal Cancer:
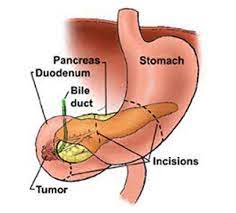
Diagnosing duodenal cancer involves a series of medical evaluations and tests. A physician will begin with a thorough medical history and physical examination. Since early symptoms are often vague, doctors may recommend further investigations like upper endoscopy, where a thin tube with a camera is inserted into the esophagus to examine the duodenum’s lining. Biopsies may be taken during endoscopy to confirm cancerous cells.
Additionally, imaging tests such as CT scans and MRI scans can provide a clearer picture of the tumor’s location, size, and spread. These diagnostic procedures collectively help stage the cancer and determine the most appropriate treatment plan.
Types and Staging:
Duodenal cancer encompasses various types, each with distinct characteristics and treatment strategies. The most common type is adenocarcinoma, arising from the glandular cells lining the duodenum. Neuroendocrine tumors, while rarer, originate from hormone-producing cells in the duodenum.
Cancer staging, ranging from stages I to IV, assesses the cancer’s size, extent of spread, and potential involvement of nearby lymph nodes or organs. Staging guides treatment decisions and provides a prognosis for individuals.
Treatment Options:
Treatment for duodenal cancer hinges on several factors, including the cancer’s stage, type, and individual health status. Surgery is often the primary approach, involving the removal of the cancerous tissue. Depending on the tumor’s size and extent, surgical options may include removing a portion of the duodenum or the entire organ.
For advanced cases or when surgery isn’t feasible, radiation therapy and chemotherapy may be recommended to shrink tumors and inhibit cancer growth. Targeted therapies, designed to target specific cancer-related proteins, are also emerging as potential treatment options.
Combining treatments, known as multimodal therapy, may be necessary for comprehensive cancer management. Consultation with a multidisciplinary team of oncologists is crucial to determining the best treatment approach.
Management and Supportive Care:
Managing duodenal cancer involves not only treating the disease but also addressing the physical and emotional well-being of individuals. Surgery and other treatments can have side effects, such as changes in digestion and potential emotional stress. Supportive care aims to alleviate these challenges and enhance quality of life.
Nutritional counseling helps individuals adapt their diets to manage post-surgery changes. Psychosocial support, including counseling and support groups, can aid emotional well-being during the cancer journey. Collaborative care ensures that individuals receive holistic support to manage both the medical and emotional aspects of their condition.
Prognosis and Survival Rates:
The prognosis for duodenal cancer varies based on factors like cancer type, stage, and treatment response. Early-stage cancers that are localized to the duodenum often have better prognoses than those that have spread to nearby lymph nodes or distant organs.
Survival rates provide an estimate of the percentage of individuals who survive a specific period after diagnosis. Keep in mind that survival rates are statistical estimates and can’t predict individual outcomes. Timely detection, effective treatment, and individual health factors significantly influence prognosis.
Preventive Measures:
While duodenal cancer’s exact cause is often elusive, certain preventive measures can help lower the risk. Adopting a healthy lifestyle that includes a balanced diet rich in fruits, vegetables, and whole grains, along with regular physical activity, can contribute to overall well-being and potentially reduce cancer risk.
Quitting smoking, limiting alcohol consumption, and managing conditions like FAP or chronic inflammation can also play a role in reducing the likelihood of developing duodenal cancer. Additionally, staying informed about family medical history can aid in identifying potential risk factors.
Frequently Asked Questions (FAQs)
Q1: What is duodenal cancer?
A1: Duodenal cancer is a type of cancer that originates in the duodenum, the first part of the small intestine. It can manifest as different types, including adenocarcinoma and neuroendocrine tumors.
Q2: What are the common symptoms of duodenal cancer?
A2: Common symptoms include abdominal discomfort, unexplained weight loss, nausea, vomiting, and changes in bowel habits. However, these symptoms can be subtle and easily confused with other gastrointestinal issues.
Q3: How is duodenal cancer diagnosed?
A3: Diagnosing duodenal cancer involves a combination of medical history, physical examination, endoscopy, biopsies, and imaging tests like CT scans or MRI scans. These tests help determine the cancer type, stage, and appropriate treatment.
Q4: What are the treatment options for duodenal cancer?
A4: Treatment options depend on factors like cancer stage and individual health. Surgery, chemotherapy, radiation therapy, and targeted therapy are common approaches. A multidisciplinary team of oncologists determines the best treatment plan.
Q5: What are the risk factors for duodenal cancer?
A5: Risk factors include genetic predisposition, inherited conditions like familial adenomatous polyposis (FAP), high-fat diets, smoking, and chronic inflammation. Family history of gastrointestinal cancers and inflammatory bowel diseases can elevate risk.
Q6: Can duodenal cancer be prevented?
A6: While exact prevention isn’t guaranteed, adopting a healthy lifestyle—such as a balanced diet, regular exercise, quitting smoking, and managing existing conditions—can reduce the risk of developing duodenal cancer.
Q7: What is the prognosis for duodenal cancer?
A7: Prognosis varies based on factors like cancer stage, type, and treatment response. Early detection and effective treatment contribute to better outcomes. Survival rates offer statistical estimates of survival but can’t predict individual outcomes.
Q8: How is duodenal cancer staged?
A8: Cancer staging involves evaluating the cancer’s size, spread, and potential involvement of lymph nodes or other organs. Staging helps guide treatment decisions and provides insights into prognosis.
Q9: What supportive care is available for duodenal cancer patients?
A9: Supportive care addresses both medical and emotional aspects of cancer. It includes nutritional counseling, psychosocial support, and strategies to manage treatment-related side effects and enhance overall well-being.
Q10: How can individuals stay informed about duodenal cancer?
A10: Staying informed involves seeking reputable medical sources, staying updated on medical advancements, and maintaining open communication with healthcare professionals. Regular check-ups and screenings can contribute to early detection.
Conclusion:
Understanding duodenal cancer is crucial for early detection, effective treatment, and proactive prevention. By recognizing potential symptoms, maintaining a healthy lifestyle, and seeking timely medical attention, individuals can make a significant impact on their well-being. Advances in medical technology and treatment options continue to offer hope for those affected by this condition. Stay informed, prioritize health, and consult healthcare professionals for personalized guidance.




