DJD (Degenerative Joint Disease): Causes, Symptoms, and Management
DJD, or Degenerative Joint Disease, is a condition that affects millions of people worldwide, often causing joint pain, stiffness, and decreased mobility. In this informative guide, we’ll explore the ins and outs of DJD, shedding light on its causes, symptoms, and effective management strategies. By gaining a deeper understanding of this common ailment, you can take proactive steps toward better joint health and an improved quality of life.
Understanding DJD
DJD, also known as osteoarthritis, is a prevalent form of arthritis that primarily affects the joints. It is characterized by the gradual degeneration of the cartilage that cushions the ends of bones in a joint.
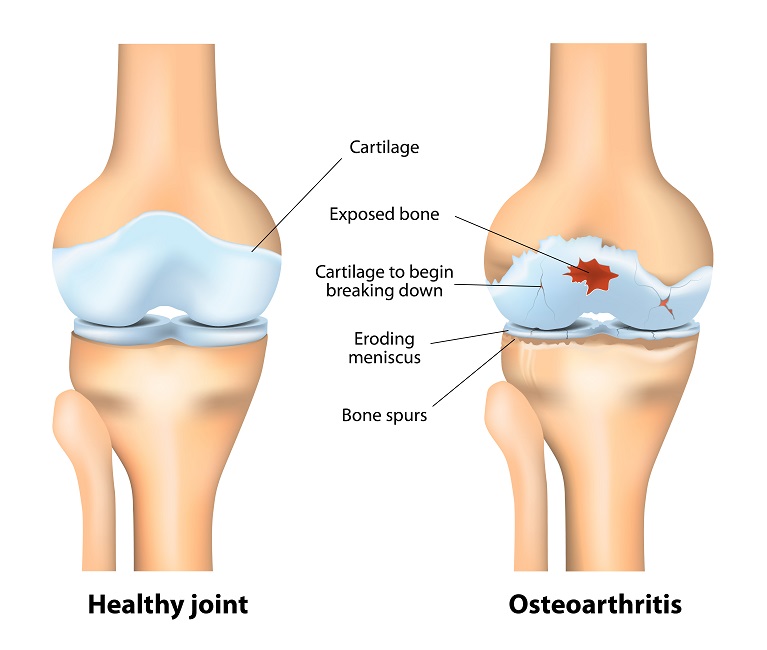
The cartilage serves as a protective barrier, preventing bone-on-bone contact and facilitating smooth joint movements. However, in individuals with DJD, this cartilage breaks down over time, leading to joint pain, inflammation, and stiffness.
Causes and Risk Factors
DJD is a complex condition with multifactorial causes. While aging is a significant contributor, several other factors can increase the risk of developing DJD.
Common Causes:
Age:
As we age, our cartilage naturally undergoes wear and tear, making it more susceptible to damage.
Joint Overuse:
Repetitive stress on a joint, often seen in athletes or those with physically demanding occupations, can accelerate cartilage degeneration.
Genetics:
Some individuals may have a genetic predisposition to DJD, making them more prone to its development.
Risk Factors:
Obesity:
Excess body weight places added stress on weight-bearing joints like the knees and hips, increasing the risk of DJD.
Joint Injuries:
Previous joint injuries or trauma can lead to localized cartilage damage and increase the likelihood of DJD.
Gender:
DJD is more common in women, particularly after menopause.
Diagnosis and Medical Evaluation
Diagnosing DJD typically involves a combination of medical history review, physical examination, and diagnostic tests. Early diagnosis is crucial for initiating effective management.
Diagnostic Methods:
Medical History:
Your healthcare provider will inquire about your symptoms, medical history, and any risk factors.
Physical Examination:
A thorough examination of the affected joint, assessing for pain, stiffness, and range of motion.
Treatment Options
The management of DJD focuses on alleviating pain, improving joint function, and enhancing the patient’s quality of life. Treatment options vary and can be tailored to individual cases.
Lifestyle Modifications:
Exercise:
Low-impact exercises like swimming or cycling can help strengthen muscles around the joint and reduce pain.
Weight Management:
Maintaining a healthy weight reduces stress on weight-bearing joints.
Joint Protection:
Techniques to protect the affected joint during daily activities can minimize strain.
Medications:
Pain Relievers:
Over-the-counter or prescription pain relievers can provide temporary relief from joint pain.
Non-steroidal anti-inflammatory Drugs (NSAIDs):
These medications help reduce pain and inflammation.
Corticosteroid Injections:
Injections into the joint can provide short-term relief from pain and inflammation.
Physical Therapy:
Physical therapists design exercise programs to improve joint strength, flexibility, and function.
Manual therapy techniques may also be employed to reduce pain and improve mobility.
Assistive Devices:
The use of braces, splints, or assistive devices can provide support to affected joints.
Surgical Intervention:
For severe cases or when conservative treatments fail, surgical procedures may be recommended. These can include joint arthroscopy, joint realignment, or joint replacement surgery.
Pain Management
Effective pain management is a critical component of DJD treatment. It helps improve the patient’s quality of life and allows them to maintain mobility.
Pain Relief Strategies:
Medications:
Prescription or over-the-counter medications can help manage pain and discomfort.
Physical Therapy:
Targeted exercises and techniques to reduce pain and improve joint function.
Lifestyle and Home Remedies
Patients with DJD can take proactive steps to manage their condition and enhance their quality of life.
Self-Care Tips:
Exercise Regularly:
Engage in low-impact exercises to strengthen muscles and maintain joint flexibility.
Healthy Diet:
Maintain a balanced diet to support overall joint health.
Joint Protection:
Practice techniques to protect your joints during daily activities.
Weight Management:
Achieve and maintain a healthy weight to reduce joint stress.
Frequently Asked Questions (FAQs)
Q1: Can DJD be prevented?
A: While DJD cannot always be prevented, maintaining a healthy weight, exercising regularly, and protecting your joints during activities can reduce the risk.
Q2: Is DJD the same as rheumatoid arthritis?
A: No, DJD is different from rheumatoid arthritis. DJD primarily involves the breakdown of joint cartilage, while rheumatoid arthritis is an autoimmune condition.
Q3: Can DJD affect any joint in the body?
A: Yes, DJD can affect any joint, but it most commonly occurs in the knees, hips, hands, and spine.
Q4: Are there alternative therapies for DJD, such as acupuncture or dietary supplements?
A: Some individuals find relief through alternative therapies, but it’s essential to consult with a healthcare professional before trying these approaches.
Q5: What are the surgical options for severe DJD?
A: Surgical interventions may include joint arthroscopy, joint realignment, or joint replacement surgery, depending on the joint affected and the severity of the condition.
Q6: Can young adults develop DJD?
A: While DJD is more common in older adults, it can occur in young adults, especially if they have joint injuries or other risk factors.
Q7: How can I manage DJD-related pain at home?
A: Managing DJD pain at home involves rest, over-the-counter pain relievers, hot and cold therapy, and following your healthcare provider’s recommendations.
Q8: Are there dietary changes that can help with DJD?
A: A balanced diet with anti-inflammatory foods may help manage DJD symptoms. Consult a nutritionist for personalized guidance.
Q9: Can physical therapy help with DJD?
A: Yes, physical therapy is a valuable part of DJD management. It focuses on strengthening muscles, improving joint function, and reducing pain.
Q10: How can I find a healthcare professional experienced in treating DJD?
A: You can start by consulting your primary care physician, who can refer you to a specialist such as a rheumatologist or orthopedic surgeon if needed.
Conclusion:
DJD, or Degenerative Joint Disease, is a widespread condition that can affect anyone, particularly as we age. While there is no cure, there are numerous treatment options and strategies for managing the pain and preserving joint function. By understanding the causes, recognizing the symptoms, and seeking early medical evaluation, individuals with DJD can take control of their joint health. With the right approach, including lifestyle modifications, pain management techniques, and a support network, it’s possible to live a fulfilling life despite the challenges posed by DJD.




