Foraminal Stenosis: Understanding Nerve Compression and Treatment Option
Foraminal stenosis is a spinal condition characterized by the narrowing of the openings (foramina) between the vertebrae, leading to compression of nerve roots. This narrowing can cause a range of symptoms, including pain, numbness, and weakness. In this comprehensive guide, we will delve into the causes, symptoms, diagnosis, and treatment options for foraminal stenosis, empowering you with knowledge to better manage this condition.
What is Foraminal Stenosis?
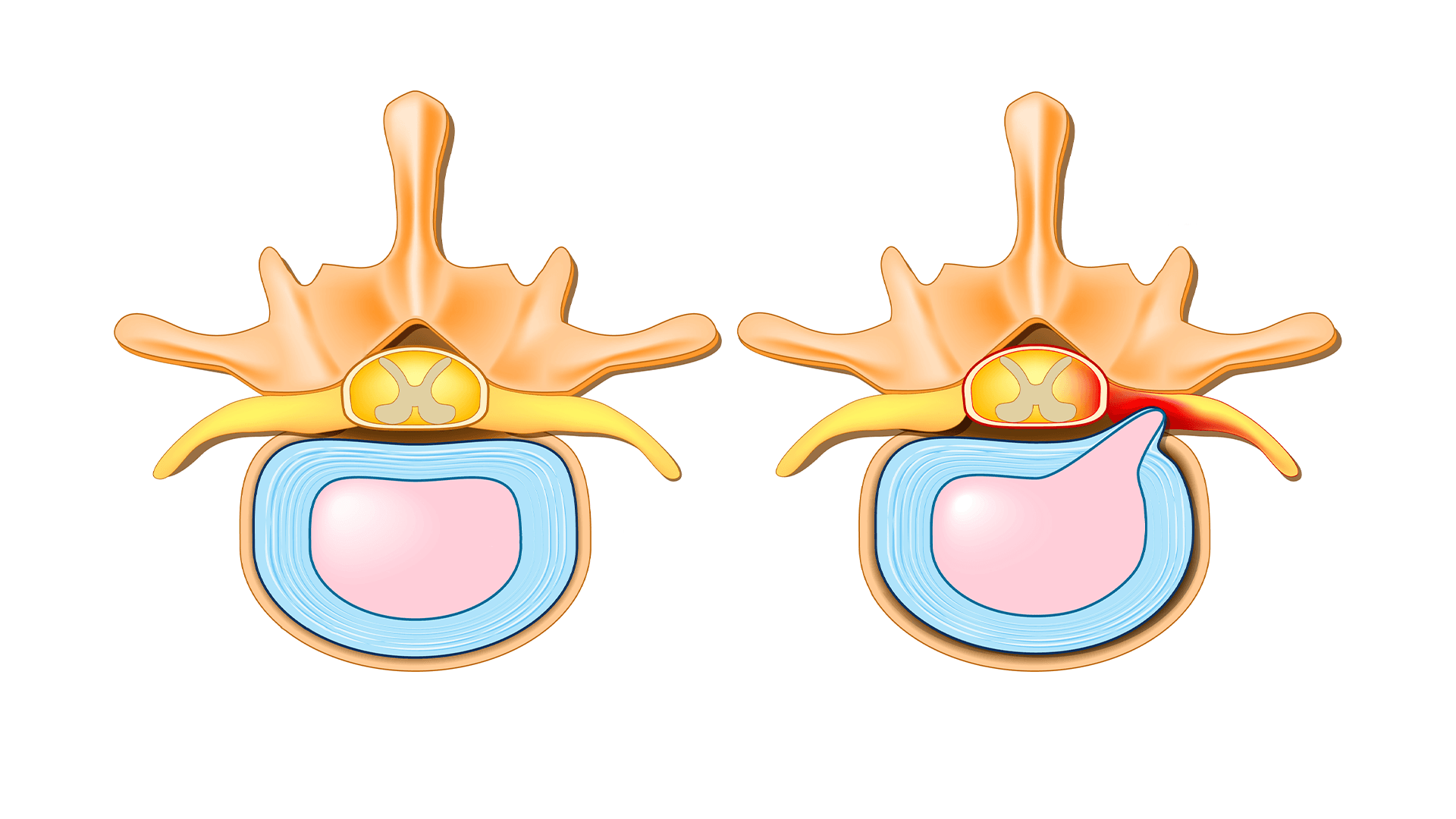
Foraminal stenosis occurs when the openings through which nerve roots exit the spinal cord become constricted. As a result, the nerves can become compressed and irritated, leading to various discomforting symptoms. The condition is often associated with degenerative changes in the spine, such as osteoarthritis and disc degeneration, which contribute to the narrowing of these openings. Understanding the mechanics of foraminal stenosis is crucial for recognizing its early signs and seeking timely medical attention.
Causes of Foraminal Stenosis
Foraminal stenosis typically develops as a result of natural wear and tear on the spine over time. Several factors contribute to its formation, including:
Degenerative Changes:
Osteoarthritis and disc degeneration can lead to the growth of bone spurs (osteophytes) and thickening of surrounding ligaments, narrowing the foramina.
Herniated Discs:
When the soft inner material of a spinal disc protrudes, it can press against the nerves, causing compression.
Facet Joint Hypertrophy:
Enlargement of the facet joints due to inflammation can reduce the space available for nerve passage.
Congenital Factors:
Some individuals may be predisposed to smaller foramina from birth, increasing their risk of developing stenosis.
By addressing these underlying causes, healthcare professionals can develop effective treatment plans tailored to each individual’s needs.
Recognizing Symptoms
Symptoms of foraminal stenosis can vary based on the location and degree of nerve compression. Common signs include:
Radicular Pain:
Shooting pain that radiates along the path of the affected nerve, often down the arm or leg.
Numbness and Tingling:
Sensations of “pins and needles” or loss of feeling in the extremities.
Muscle Weakness:
Reduced strength or control in specific muscle groups.
Aggravated Pain:
Symptoms may worsen with certain movements, positions, or activities.
Recognizing these symptoms is essential for seeking timely medical evaluation and intervention. Left untreated, foraminal stenosis can lead to further complications and decreased quality of life.
Diagnosis and Medical Evaluation
If you experience symptoms suggestive of foraminal stenosis, seeking medical attention is crucial. A healthcare provider will perform a comprehensive evaluation, which may include:
Physical Examination:
Assessing your range of motion, reflexes, and muscle strength.
Neurological Tests:
Evaluating nerve function and responsiveness.
Imaging Studies:
X-rays, MRI scans, or CT scans to visualize the spine and identify narrowing or compression.
Diagnostic Injections:
Injecting a local anesthetic near the affected nerve to confirm the source of pain.
Taking Control of Your Spinal Health
Understanding the mechanics of foraminal stenosis and recognizing its early symptoms are crucial first steps. By becoming aware of the factors that contribute to its development, you can make informed decisions that positively impact your spinal health. Whether it’s degenerative changes, herniated discs, or facet joint hypertrophy, addressing these underlying causes can play a pivotal role in preventing and managing foraminal stenosis.
Seeking Timely Medical Evaluation
If you experience symptoms such as radicular pain, numbness, tingling, or muscle weakness, seeking prompt medical attention is vital. A comprehensive evaluation, including physical examination, neurological tests, and imaging studies, can lead to an accurate diagnosis. The sooner you obtain a precise diagnosis, the sooner you can embark on an appropriate treatment journey tailored to your unique condition.
Exploring Treatment Options
Treatment for foraminal stenosis spans a spectrum of approaches, each aimed at relieving discomfort and enhancing your quality of life. From conservative measures such as physical therapy, pain management, and lifestyle adjustments to interventional procedures like epidural steroid injections and nerve root blocks, there are diverse paths to consider. In cases where conservative measures prove insufficient, surgical intervention, such as laminectomy or foraminotomy, may be explored.
Embracing a Healthy Lifestyle
Managing foraminal stenosis extends beyond medical interventions. Embracing a healthy lifestyle that includes regular exercise, maintaining proper posture, and adhering to a balanced diet can significantly contribute to your spinal health. By incorporating these habits into your daily routine, you can reduce the risk of further degeneration and enhance your overall well-being.
Frequently Asked Questions (FAQs) About Foraminal Stenosis
1. What is foraminal stenosis?
Foraminal stenosis is a spinal condition characterized by the narrowing of the openings (foramina) between the vertebrae, leading to compression of nerve roots.
2. What causes foraminal stenosis?
Foraminal stenosis is primarily caused by degenerative changes in the spine, such as osteoarthritis, herniated discs, facet joint hypertrophy, and congenital factors.
3. What are the symptoms of foraminal stenosis?
Common symptoms include radicular pain, numbness, tingling, and muscle weakness along the affected nerve pathways.
4. How is foraminal stenosis diagnosed?
Diagnosis involves physical examination, neurological tests, and imaging studies such as X-rays, MRI scans, and CT scans to visualize spinal structures.
5. Can foraminal stenosis be prevented?
While it may not be completely preventable, maintaining a healthy lifestyle, practicing proper posture, and avoiding excessive strain on the spine can help reduce the risk.
6. What are the treatment options for foraminal stenosis?
Treatment can range from conservative measures like physical therapy and pain management to interventional procedures such as epidural steroid injections. Surgical options like laminectomy or foraminotomy may be considered in severe cases.
7. How can physical therapy help with foraminal stenosis?
Physical therapy aims to improve mobility, strength, and flexibility, alleviating symptoms and enhancing overall spinal health.
8. Are there non-surgical treatments for foraminal stenosis?
Yes, non-surgical treatments include pain medications, anti-inflammatory drugs, epidural injections, and lifestyle modifications.
9. Is surgery always necessary for foraminal stenosis?
No, surgery is typically considered after conservative treatments have been exhausted. It’s important to consult a medical professional for personalized recommendations.
10. What is the recovery process after surgery for foraminal stenosis?
Recovery varies based on the type of surgery. Physical therapy and rehabilitation play a crucial role in regaining strength and mobility.
Conclusion
Our journey through the intricacies of foraminal stenosis has equipped us with a deep understanding of this spinal condition. From its underlying causes to its potential treatment avenues, we have delved into the realm of nerve compression and explored strategies for enhancing your quality of life.




