Understanding Gastroschisis: A Comprehensive Guide
Gastroschisis is a rare congenital condition that affects abdominal wall development in infants. In this comprehensive guide, we’ll delve into the causes, symptoms, and treatment options available for babies born with gastroschisis.
What is Gastroschisis?
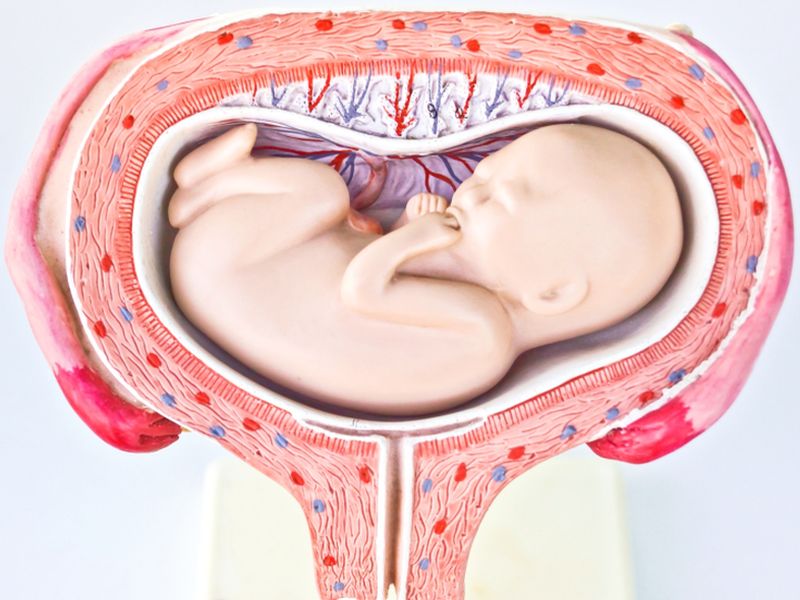
Gastroschisis is a birth defect where an infant is born with their intestines and sometimes other organs outside of the body, due to a hole in the abdominal wall. This condition occurs early in fetal development and is usually detected during prenatal ultrasounds.
Gastroschisis is distinct from omphalocele, another abdominal wall defect where organs are covered by a protective sac. In gastroschisis, the exposed organs are in direct contact with the amniotic fluid, which can lead to various complications.
Causes and Risk Factors
The exact cause of gastroschisis is not fully understood, but research suggests a combination of genetic and environmental factors. While the condition can’t always be prevented, certain risk factors have been identified. Young maternal age, tobacco use, and drug abuse during pregnancy have been linked to an increased risk of gastroschisis.
Recent studies have also explored potential associations between gastroschisis and specific genetic variations. However, more research is needed to establish definitive links.
Symptoms and Diagnosis
Infants born with gastroschisis exhibit visible symptoms immediately after birth. The exposed intestines and organs are evident on the baby’s abdominal area. Other symptoms may include a swollen belly, difficulty feeding, and breathing problems.
Diagnosis is typically confirmed through prenatal ultrasounds, which can detect the condition before birth. After delivery, a physical examination and imaging tests help assess the extent of the condition and plan appropriate treatment.
Treatment Options
Prompt and effective treatment is crucial for infants born with gastroschisis. The primary goal is to carefully return the exposed organs into the abdomen and repair the abdominal wall. Treatment typically involves the following steps:
Surgical Correction:
The exposed organs are gently placed back into the abdominal cavity, and the abdominal wall defect is surgically closed. The timing of surgery depends on the baby’s overall health and stability.
Close Monitoring:
After surgery, babies require intensive care and monitoring in a neonatal intensive care unit (NICU). The medical team assesses the baby’s progress and ensures that the repaired abdominal wall heals properly.
Nutritional Support:
Babies with gastroschisis may initially have difficulty with feeding due to the stress on their digestive system. They might receive nutrition through intravenous (IV) fluids or a feeding tube until they can tolerate oral feedings.
Potential Complications:
While most infants recover well, complications such as infection, intestinal issues, or developmental delays can arise. Regular check-ups and follow-ups are essential to monitor the baby’s growth and development.
Preparing for Surgery and Recovery
Preparing for surgery and understanding the recovery process are essential steps for families navigating the challenges of gastroschisis. Here’s what parents and caregivers can expect:
Preoperative Planning:
Before surgery, medical teams will thoroughly assess the baby’s condition. Parents will receive information about the procedure, potential risks, and expected outcomes. Clear communication between medical professionals and families is key.
Surgical Procedure:
The surgical correction of gastroschisis involves carefully placing the exposed organs back into the abdomen and repairing the abdominal wall defect. Surgeons work diligently to ensure a successful closure.
Post-Op Care:
Following surgery, babies require close monitoring in the NICU. The medical team will assess vital signs, incision healing, and bowel function. Pain management and infection prevention are also priorities.
Feeding Progression:
Infants may start with IV nutrition and gradually transition to oral feedings as their digestive system recovers. Healthcare professionals guide parents on feeding schedules and techniques.
Incision Care:
Proper care of the surgical incision site is crucial to prevent infection. Medical staff will provide instructions on how to clean and care for the incision, as well as signs of infection to watch for.
Long-Term Follow-Up:
Babies who undergo gastroschisis repair need regular check-ups to monitor growth and development. Long-term complications, if any, are addressed promptly.
Long-Term Outlook and Potential Complications
While many babies with gastroschisis go on to lead healthy lives after successful treatment, there are potential long-term considerations and complications to be aware of:
Bowel Function:
Babies who underwent surgery for gastroschisis might experience challenges with bowel function. Some may require ongoing medical management, dietary adjustments, or additional surgeries.
Developmental Milestones:
Babies born with gastroschisis might reach developmental milestones at a slightly different pace. Early intervention services, such as physical therapy and occupational therapy, can help address any delays.
Adhesions:
Surgical repairs can sometimes lead to adhesions, where tissues stick together. Adhesions might cause discomfort or bowel obstruction and may require further medical attention.
Nutrition and Growth:
Ensuring proper nutrition and growth is crucial for babies with gastroschisis. Some infants may need specialized feeding plans or nutritional supplements to support healthy growth.
Psychosocial Support:
Families of babies with gastroschisis may encounter emotional and psychosocial challenges. Connecting with support groups, counseling services, and other families can provide valuable reassurance.
Regular medical follow-ups and open communication with healthcare providers are essential to address potential complications promptly. While each child’s journey is unique, early intervention and ongoing care can significantly enhance their quality of life.
Support and Resources for Families
Families of babies with gastroschisis are not alone. Numerous organizations, online communities, and support groups provide a space for parents to connect, share experiences, and access valuable resources. These platforms offer emotional support, information about the latest research, and guidance from families who have been through similar journeys.
Advances in Research and Treatment
The medical field is continually advancing, and researchers are dedicated to improving the outcomes for babies born with gastroschisis. Some recent developments and areas of research include:
Minimally Invasive Surgery:
Advancements in surgical techniques are leading to less invasive approaches for repairing abdominal wall defects. These techniques aim to reduce scarring and improve recovery times.
Fetal Intervention:
Researchers are exploring the possibility of treating gastroschisis in utero, before birth. Fetal surgeries may help prevent damage to the exposed organs and improve outcomes.
Long-Term Follow-Up Studies:
Long-term studies are tracking the progress of children who have undergone gastroschisis repair. These studies provide insights into the challenges they may face as they grow and help refine treatment approaches.
Nutritional Strategies:
Nutritional management for infants with gastroschisis is an active area of research. Finding the optimal feeding strategies to support growth and development remains a priority.
Genetic Studies:
Research into the genetic factors contributing to gastroschisis is ongoing. Understanding the genetic basis of the condition may pave the way for early detection and personalized treatments.
Empowering Families with Knowledge
Families affected by gastroschisis play a vital role in raising awareness and advocating for their children’s health. By staying informed about the latest research and treatment options, parents can actively participate in decisions related to their child’s care.
Frequently Asked Questions (FAQs) About Gastroschisis
1. What is gastroschisis?
Gastroschisis is a birth defect where an infant is born with intestines and sometimes other organs outside the body due to a hole in the abdominal wall.
2. How is gastroschisis diagnosed?
Gastroschisis is often detected through prenatal ultrasounds. After birth, a physical examination and imaging tests confirm the condition.
3. What causes gastroschisis?
While the exact cause is unclear, a combination of genetic and environmental factors may contribute to the development of gastroschisis.
4. Can gastroschisis be treated?
Yes, gastroschisis can be treated through surgical correction. The exposed organs are carefully placed back into the abdomen, and the abdominal wall is repaired.
5. What is the recovery process like after surgery?
After surgery, infants require close monitoring in the neonatal intensive care unit (NICU). Feeding progression, incision care, and post-operative check-ups are important aspects of recovery.
6. Are there potential complications associated with gastroschisis?
Yes, potential complications include challenges with bowel function, developmental delays, adhesions, and growth concerns. Regular medical follow-ups help address these issues.
7. Are there long-term effects of gastroschisis?
Some children may experience long-term effects related to bowel function, growth, and development. Early intervention services can help address these concerns.
8. Is there ongoing research into gastroschisis?
Yes, ongoing research aims to improve treatment outcomes and advance understanding of the condition. Minimally invasive surgery, fetal interventions, and genetic studies are areas of focus.
9. How can families find support for gastroschisis?
Families can connect with online communities, support groups, and organizations dedicated to gastroschisis. These platforms offer resources, information, and a space to share experiences.
10. What should parents do if their child is diagnosed with gastroschisis?
If your child is diagnosed with gastroschisis, seek guidance from medical professionals. Stay informed, connect with support networks, and collaborate with your healthcare team for the best care.
Conclusion
The journey of gastroschisis is one that requires resilience, support, and access to accurate information. Understanding the causes, symptoms, treatment options, and potential challenges empowers families to make informed decisions for their infants’ well-being.




