Miller Fisher Syndrome: Symptoms, Diagnosis, and Treatment
Miller Fisher Syndrome (MFS) is a rare neurological disorder that falls under the umbrella of Guillain-Barré Syndrome (GBS). While it’s uncommon, understanding MFS is crucial as early detection can lead to better outcomes. In this comprehensive guide, we delve into the intricacies of Miller Fisher Syndrome, exploring its causes, symptoms, diagnosis, and treatment options.
What Causes Miller Fisher Syndrome?
The exact cause of Miller Fisher Syndrome remains under study, but it is believed to be triggered by an abnormal immune system response. This response often follows a recent infection, commonly with viruses like the Epstein-Barr virus or certain bacteria. While the precise mechanisms are still being investigated, this autoimmune aspect distinguishes MFS from other neurological conditions.
Symptoms of Miller Fisher Syndrome
Recognizing the symptoms of Miller Fisher Syndrome is critical for early diagnosis. This condition is characterized by a triad of distinctive symptoms:
Ataxia
Ataxia refers to a lack of muscle coordination, leading to unsteady movements and difficulties with balance. In MFS, ataxia is often one of the initial symptoms and can be alarming for those affected.
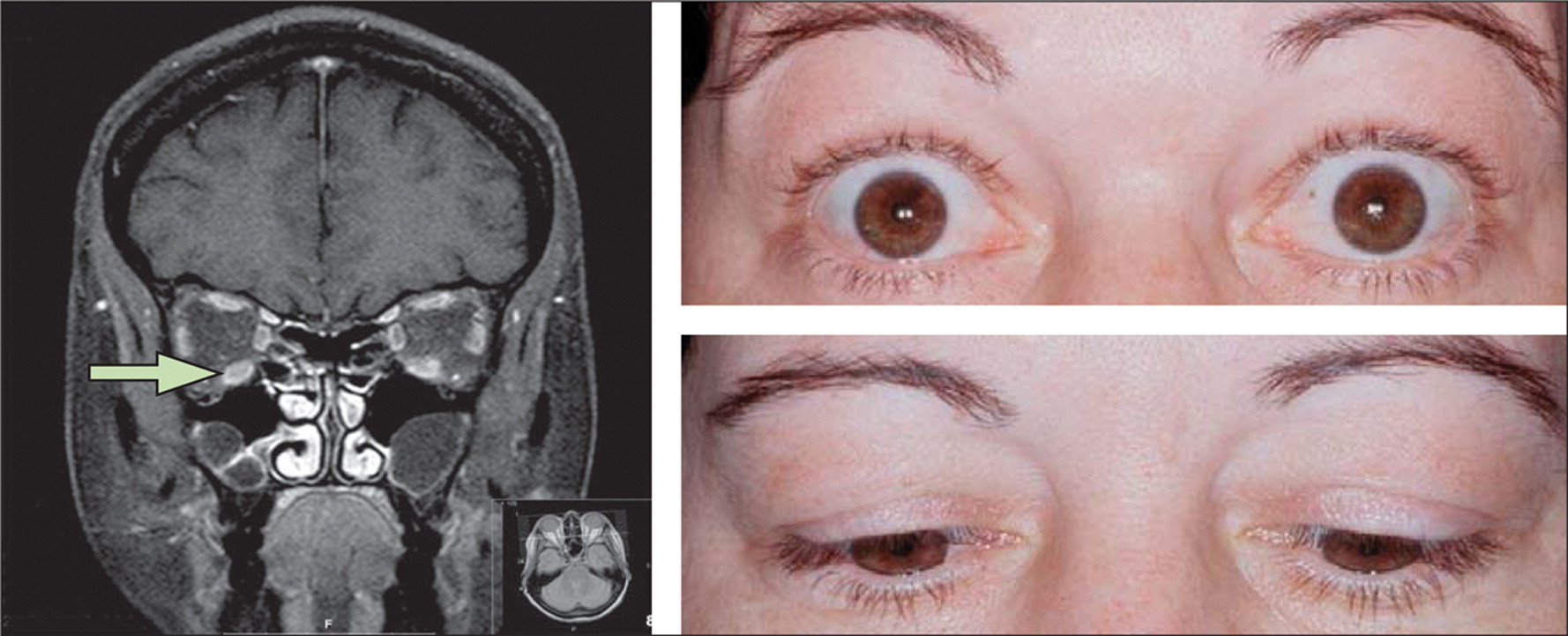
Ophthalmoplegia
Ophthalmoplegia refers to weakness or paralysis of the eye muscles, causing double vision, difficulty moving the eyes, and drooping eyelids. It is a hallmark symptom of MFS and is often accompanied by ptosis (eyelid drooping).
Areflexia
Areflexia means the absence of reflexes, particularly deep tendon reflexes like the knee-jerk reflex. In MFS, areflexia in combination with ataxia and ophthalmoplegia forms the classic triad, aiding in diagnosis.
Diagnosis and Medical Evaluation
Diagnosing Miller Fisher Syndrome involves a thorough medical evaluation. Healthcare professionals will consider the patient’s medical history and conduct various tests, including:
Clinical Assessments
During a clinical examination, the healthcare provider will assess the patient’s neurological functions, looking for the characteristic triad of ataxia, ophthalmoplegia, and areflexia. This clinical evaluation is a crucial initial step in diagnosing MFS.
Cerebrospinal Fluid Analysis
A lumbar puncture, also known as a spinal tap, may be performed to analyze the cerebrospinal fluid. Elevated protein levels in the cerebrospinal fluid can provide supporting evidence for an MFS diagnosis.
Nerve Conduction Studies
Nerve conduction studies and electromyography (EMG) can help assess nerve function and confirm the presence of demyelination, which is common in MFS.
Miller Fisher Syndrome vs. Guillain-Barré Syndrome
Miller Fisher Syndrome is often grouped under Guillain-Barré Syndrome, but they have distinct characteristics:
Miller Fisher Syndrome (MFS)
Characterized by the triad of ataxia, ophthalmoplegia, and areflexia.
Generally presents with cranial nerve involvement.
Rarely causes significant limb weakness.
Excellent recovery prognosis with early treatment.
Guillain-Barré Syndrome (GBS)
Primarily involves limb weakness and can lead to muscle paralysis.
Absence of ataxia and ophthalmoplegia in most cases.
May require more extensive medical intervention.
Recovery prognosis varies, and some cases may have residual weakness.
Understanding these differences is crucial, as it impacts the approach to treatment and prognosis.
Treatment and Management
Early intervention is key to managing Miller Fisher Syndrome effectively:
Intravenous Immunoglobulin (IVIG) or Plasma Exchange
Treatment often involves IVIG therapy or plasma exchange, which helps modulate the immune response and reduce the severity of symptoms. These treatments are most effective when administered promptly after diagnosis.
Supportive Care
In addition to specific treatments, patients may require supportive care to address individual symptoms. This can include physical therapy for ataxia or treatments to manage double vision.
Prognosis and Recovery
The prognosis for individuals with Miller Fisher Syndrome is generally positive, especially with early treatment:
Positive Outcomes
Many patients experience significant improvement within weeks to months after treatment initiation. Some may achieve a full recovery.
Residual Symptoms
In some cases, individuals may have residual symptoms such as mild weakness or ocular issues, but these are often manageable.
Follow-up Care
Regular follow-up care with healthcare providers is essential to monitor progress and address any lingering symptoms.
Coping with Miller Fisher Syndrome
Coping with Miller Fisher Syndrome involves both medical and emotional support:
Emotional Well-being
Dealing with a neurological condition can be emotionally challenging. It’s essential to seek emotional support from friends, family, or support groups to navigate these challenges.
Lifestyle Adjustments
Patients may need to make lifestyle adjustments during their recovery. This can include adapting to new physical limitations or addressing changes in daily routines.
Research and Future Developments
Ongoing research is advancing our understanding of Miller Fisher Syndrome:
Promising Research
Researchers continue to investigate the underlying mechanisms of MFS and potential new treatment approaches. Stay updated on the latest developments.
Support and Resources
Support and resources are available for individuals and families affected by Miller Fisher Syndrome:
Support Groups
Joining support groups or online communities can provide valuable insights, shared experiences, and emotional support.
Reliable Resources
Explore reputable sources such as medical associations and research organizations for up-to-date information on Miller Fisher Syndrome.
Frequently Asked Questions (FAQs) About Miller Fisher Syndrome
What is Miller Fisher Syndrome (MFS)?
Miller Fisher Syndrome (MFS) is a rare neurological disorder characterized by a triad of symptoms: ataxia, ophthalmoplegia, and areflexia. It’s considered a variant of Guillain-Barré Syndrome (GBS).
How common is Miller Fisher Syndrome?
MFS is quite rare, accounting for about 1-5% of all GBS cases. It’s estimated to occur in 1 in every 1,000,000 people annually.
What causes Miller Fisher Syndrome?
The exact cause of MFS is not fully understood, but it is believed to be triggered by an abnormal immune response following infections, often viral or bacterial.
What are the typical symptoms of Miller Fisher Syndrome?
The hallmark symptoms of MFS include ataxia (lack of muscle coordination), ophthalmoplegia (eye muscle weakness), and areflexia (absence of reflexes). These symptoms often occur together.
How is Miller Fisher Syndrome diagnosed?
Diagnosis involves clinical evaluations, cerebrospinal fluid analysis, and nerve conduction studies. These tests help confirm the presence of MFS and rule out other conditions.
Is Miller Fisher Syndrome treatable?
Yes, MFS is treatable. Early intervention with therapies like intravenous immunoglobulin (IVIG) or plasma exchange can lead to significant improvement in symptoms.
Are there any long-term complications associated with MFS?
While many individuals with MFS recover fully, some may experience residual symptoms or minor neurological issues. Regular follow-up care is essential.
Can Miller Fisher Syndrome recur?
Recurrence is rare but possible. If it does recur, it typically presents with milder symptoms than the initial episode.
Are there support groups for individuals with MFS?
Yes, there are support groups and online communities where individuals and families affected by MFS can connect, share experiences, and find emotional support.
Is there ongoing research on Miller Fisher Syndrome?
Yes, ongoing research aims to better understand the underlying mechanisms of MFS and develop more effective treatments. Staying informed about research developments is essential.
Conclusion:
In conclusion, Miller Fisher Syndrome is a rare but treatable neurological disorder characterized by the triad of ataxia, ophthalmoplegia, and areflexia. Early diagnosis and appropriate treatment can lead to positive outcomes and recovery. If you or a loved one suspect MFS, seek medical evaluation promptly. Remember that support, both medical and emotional, plays a significant role in managing this condition. Stay informed about the latest research and resources to enhance your journey toward recovery.




