Understanding the long-term consequences of head injuries and related conditions like epilepsy is crucial for patient care and public health initiatives. A recent study published in JAMA Neurology sheds light on the association between post-traumatic epilepsy (PTE) and an increased risk of developing dementia later in life.
Understanding Post-Traumatic Epilepsy (PTE)
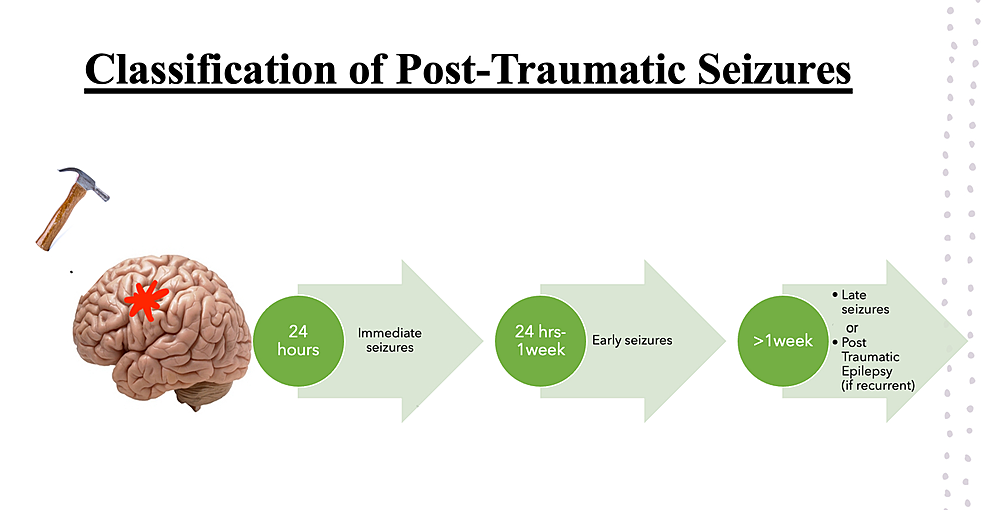
PTE is a specific type of epilepsy diagnosed when someone develops unprovoked seizures more than a week after sustaining a head injury. It accounts for roughly 5-20% of all acquired epilepsy cases, highlighting its significance as a potential long-term consequence of head trauma.
Previous Research and Unanswered Questions
While previous research has established associations between head injuries and epilepsy, and both conditions are known independent risk factors for dementia, a critical gap existed in understanding the long-term cognitive outcomes specifically for individuals with PTE. This new study aims to address this knowledge gap.
Study Design and Methodology
The researchers used data from the Atherosclerosis Risk in Communities (ARIC) study, a large, community-based, long-term investigation spanning over 30 years. This provided valuable insights into the health outcomes of a diverse population over an extended period.
The study compared the risk of developing dementia among individuals with PTE to three other groups:
- Head injury only
- No head injury or seizure/epilepsy
- Seizure/epilepsy only
The primary hypothesis was that PTE would be associated with a much higher risk of dementia compared to either head injury or seizure/epilepsy alone. Additionally, the researchers explored potential variations in the association based on factors like:
- Race
- Sex
- Age
- Head injury severity and frequency
Key Findings and Insights
The study revealed several crucial findings:
- Increased Dementia Risk: Individuals with PTE displayed an approximately 4.5-fold increase in dementia risk compared to those with no history of epilepsy or head injury.
- Accounting for Competing Risks: Even after considering the potential influence of other factors like stroke and mortality, the dementia risk associated with PTE remained around 3 times higher.
- Significance Compared to Other Factors: The study showed that the PTE-associated dementia risk was significantly higher than the risk associated with either head injury alone or seizure/epilepsy alone.
- Long-Term Impact: The findings highlight the long-term consequences of PTE, emphasizing the importance of not just preventing head injuries but also taking steps to minimize the risk of developing PTE after a head injury.
Additional Observations and Study Strengths
The study offers valuable insights beyond its core findings:
- Large Sample Size and Long-Term Follow-Up: Utilizing a large, community-based sample followed for up to 30 years strengthens the study’s generalizability and reliability.
- Mean Participant Age: The average participant age being 54 years is relevant considering the higher prevalence of epilepsy and head injuries in older individuals.
- Age-Specific Risk Variations: The study observed a higher relative risk of PTE-associated dementia in younger individuals compared to older individuals. This could be due to a higher likelihood of older individuals with PTE dying before receiving a dementia diagnosis.
- No Significant Race or Sex Interaction: The study revealed no significant influence of race or sex on the observed associations.
- Impact of Head Injury Severity: No significant differences were observed in dementia risk between cases of PTE following first or second head injuries, or between mild versus moderate/severe injuries.
Limitations and Future Research Directions
While valuable, the study acknowledges some limitations:
- Sample Bias: The study population consisted of older adults with no prior head injury at baseline, limiting the generalizability to individuals who experience head injuries earlier in life.
- Unaccounted Factors: Potential confounding factors like physical functioning and frailty were not considered.
- Limited Head Injury Data: The study relied on self-reported data regarding head injuries, which may not capture the full extent of mild injuries.
- Data Availability: Information on crucial variables like clinical characteristics, injury mechanisms, and acute imaging findings was unavailable.
- Limited Seizure/Epilepsy Data: The study defined seizure/epilepsy and PTE based on ICD-9/10 codes due to the lack of a self-reported seizure/epilepsy measure at baseline, potentially affecting the precision of the analysis.
Moving forward, research should explore these limitations and delve deeper into:
- Underlying Mechanisms: Identifying the biological and neurodegenerative processes that contribute to the link between PTE and dementia risk.
- Risk Factor Identification: Investigating individual and environmental factors that may increase the risk of developing PTE after a head injury.
- Prevention Strategies: Developing effective strategies to prevent both




