The Enigma: Right-Sided Heart Failure
Right-sided heart failure is a condition that affects the ability of the right side of the heart to pump blood effectively. It is an important topic to understand as it can have significant implications for a person’s overall health and well-being. In this article, we will delve into the anatomy and physiology of the heart, explore the mechanisms and pathophysiology of right-sided heart failure, and discuss its clinical presentation and diagnosis, as well as treatment and management approaches. We will also touch upon the potential complications and prognosis, provide preventive tips, and address frequently asked questions. By shedding light on this condition, we hope to raise awareness and promote early detection and proper management ofright-sidedd heart failure.
Anatomy and Physiology of the Heart
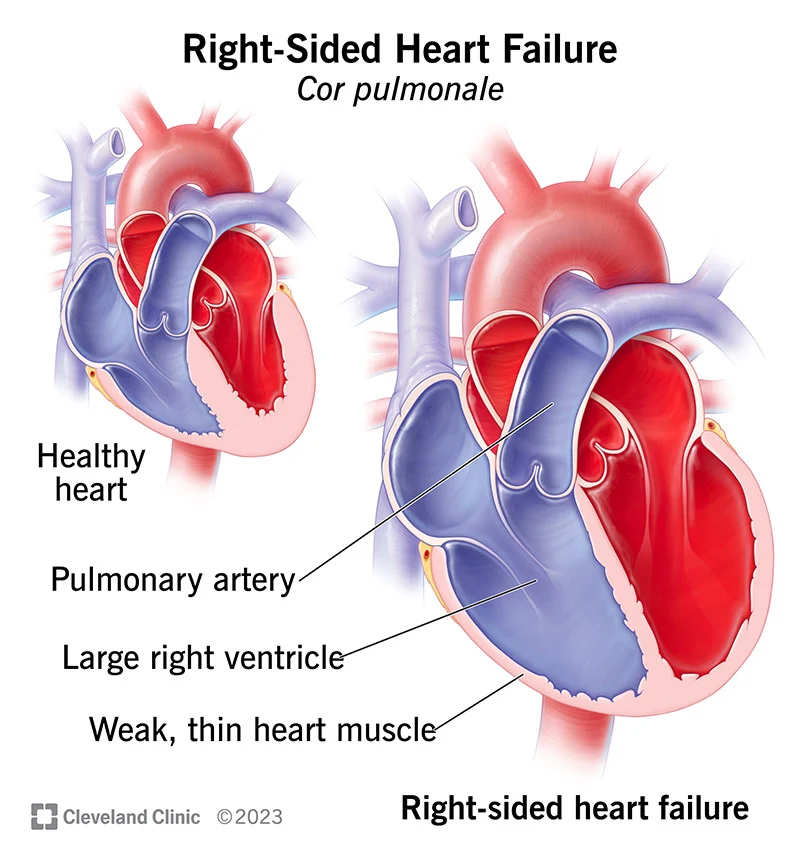
The heart plays a crucial role in the circulatory system, pumping oxygen-rich blood to the body’s tissues and organs. It consists of four chambers: two atria (left and right) and two ventricles (left and right). The right side of the heart receives deoxygenated blood from the body’s tissues and pumps it to the lungs for oxygenation. Right-sided heart failure occurs when the right ventricle is unable to effectively pump blood, leading to a backup of blood in the veins and fluid accumulation in the body’s tissues. This can occur due to various reasons, including underlying heart conditions, such as left-sided heart failure, pulmonary hypertension, or heart valve disorders.
Understanding Heart Failure
Heart failure is a condition where the heart’s ability to pump blood is impaired. It can be categorized into left-sided heart failure and right-sided heart failure, depending on the affected side of the heart. Right-sided heart failure specifically refers to the inability of the right side of the heart to pump blood efficiently. It often occurs as a result of left-sided heart failure, where the weakened left ventricle causes increased pressure and fluid buildup in the lungs, leading to strain on the right side of the heart. Other causes of right-sided heart failure include pulmonary hypertension (high blood pressure in the lungs), heart valve diseases, congenital heart defects, and chronic lung diseases.
The symptoms of right-sided heart failure may include fatigue, swelling in the legs and ankles (edema), fluid retention in the abdomen (ascites), and shortness of breath. Risk factors for developing right-sided heart failure include a history of heart disease, high blood pressure, obesity, diabetes, and smoking.
Additionally, conditions that directly affect the right side of the heart can also contribute to tonight-sided heart failure. Pulmonary hypertension, for example, is a condition characterized by high blood pressure in the lungs. This increased pressure puts strain on the right ventricle, impairing its ability to pump blood efficiently. Heart valve diseases, such as tricuspid regurgitation or stenosis, can also affect the right side of the heart and lead to right-sided heart failure.
Certain congenital heart defects, such as atrial septal defect or ventricular septal defect, can cause communication between the left and right sides of the heart, leading to increased blood flow and pressure on the right side, eventually resulting in right-sided heart failure. Chronic lung diseases, such as chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis, can also exert pressure on the right side of the heart, causing it to weaken over time.
Clinical Presentation and Diagnosis
The clinical presentation of right-sided heart failure can vary depending on the severity of the condition. Common symptoms include fatigue, swelling in the lower extremities (edema), fluid retention in the abdomen (ascites), and shortness of breath, especially during physical activity or when lying flat (orthopnea).
Diagnosing right-sided heart failure involves a comprehensive evaluation of the patient’s medical history, physical examination, and diagnostic tests. The healthcare provider will inquire about the symptoms experienced, risk factors, and any previous heart conditions. During the physical examination, they may look for signs of fluid retention, such as swollen ankles and distended neck veins.
Diagnostic tests commonly used to identify right-sided heart failure include:
Echocardiogram:
This non-invasive test uses sound waves to create images of the heart and assess its structure and function. It can help determine the size and function of the right ventricle and detect any abnormalities.
Electrocardiogram (ECG):
An ECG measures the electrical activity of the heart and can provide information about any rhythm abnormalities or signs of right ventricular strain.
Chest X-ray:
A chest X-ray can reveal signs of fluid buildup in the lungs or an enlarged heart, which may indicate right-sided heart failure.
Blood tests:
Blood tests may be conducted to assess kidney and liver function, as well as check for elevated levels of certain biomarkers associated with heart failure.
Cardiac catheterization:
In some cases, a cardiac catheterization may be performed to measure pressures within the heart chambers and assess blood flow.
Treatment and Management Approaches
The primary goals of treating right-sided heart failure are to improve symptoms, slow disease progression, and enhance the patient’s quality of life. The specific treatment approach will depend on the underlying cause and severity of the condition. Treatment options for right-sided heart failure may include:
Medications:
Several medications can be prescribed to manage right-sided heart failure. Diuretics help reduce fluid retention and relieve symptoms of edema. ACE inhibitors or angiotensin receptor blockers (ARBs) may be used to dilate blood vessels and lower blood pressure. In some cases, beta-blockers or inotropic agents may be prescribed to improve heart function and reduce symptoms.
Lifestyle modifications:
Making certain lifestyle changes can significantly improve the management of right-sided heart failure. Patients are often advised to follow a low-sodium diet to reduce fluid retention. Regular exercise, as recommended by a healthcare professional, can help strengthen the heart and improve overall cardiovascular health. Quitting smoking and limiting alcohol consumption are also important steps in managing the condition.
Fluid and salt restriction:
Limiting fluid intake and reducing salt consumption can help prevent fluid overload and minimize symptoms of right-sided heart failure.
Oxygen therapy: In cases where oxygen levels are low, supplemental oxygen therapy may be prescribed to improve breathing and oxygenation of the blood.
Device therapy:
In some advanced cases, device therapy such as cardiac resynchronization therapy (CRT) or implantable cardioverter-defibrillators (ICDs) may be recommended to help regulate heart rhythm and improve cardiac function.
Surgical interventions:
In severe cases, of of right-sided heart failure, surgical interventions such as heart valve repair or replacement, coronary artery bypass grafting (CABG), or ventricular assist device (VAD) implantation may be considered.
Complications and Prognosis
Untreated or poorly managed right-sided heart failure can lead to several complications, including:
Fluid buildup:
The accumulation of fluid in the lungs (pulmonary edema) can cause severe breathing difficulties and increase the risk of respiratory infections.
Organ damage:
Inadequate blood flow and oxygenation can affect the function of vital organs, such as the kidneys and liver, leading to organ damage or failure.
Arrhythmias:
The weakened heart muscle and altered electrical conduction can result in abnormal heart rhythms, which can be life-threatening.
Right-sided heart enlargement:
Prolonged right-sided heart failure can cause the right ventricle to enlarge, further impairing its ability to pump blood effectively.
FAQ’s
What are the common symptoms of right-sided heart failure?
Common symptoms of right-sided heart failure include fatigue, swelling in the legs and ankles (edema), fluid retention in the abdomen (ascites), and shortness of breath.
Can right-sided heart failure occur without any underlying heart conditions?
While right-sided heart failure often occurs as a result of left-sided heart failure or other heart conditions, it can also be caused by pulmonary hypertension, heart valve diseases, congenital heart defects, or chronic lung diseases.
How is right-sided heart failure diagnosed?
Diagnosis of right-sided heart failure involves a comprehensive evaluation of the patient’s medical history, physical examination, and diagnostic tests such as an echocardiogram, electrocardiogram (ECG), chest X-ray, and blood tests.
Are there any specific medications used to treat right-sided heart failure?
Medications commonly used to treat right-sided heart failure include diuretics, ACE inhibitors or ARBs, beta-blockers, and inotropic agents. The specific medication regimen will depend on the individual’s condition and underlying causes.
Can lifestyle changes alone improve right-sided heart failure?
Lifestyle changes, such as following a low-sodium diet, engaging in regular exercise, quitting smoking, and limiting alcohol consumption, can significantly improve the management of right-sided heart failure. However, medical treatment and close monitoring are often necessary.
Are there any dietary restrictions for individuals with right-sided heart failure?
Individuals with right-sided heart failure are often advised to follow a low-sodium diet to reduce fluid retention. It is important to consult with a healthcare professional or registered dietitian for personalized dietary recommendations.
Can right-sided heart failure be reversed or cured completely?
While right-sided heart failure cannot be completely cured, it can be effectively managed with appropriate treatment and lifestyle modifications. Early detection and proper management can slow disease progression and improve symptoms.
What are the potential complications of untreated right-sided heart failure?
Untreated or poorly managed right-sided heart failure can lead to complications such as fluid buildup in the lungs(pulmonary edema), organ damage, arrhythmias, and right-sided heart enlargement.
Are there any ongoing research or advancements in the treatment of right-sided heart failure?
Yes, there is ongoing research and advancements in the treatment of right-sided heart failure. These include new medications, surgical techniques, and device therapies that aim to improve outcomes and quality of life for individuals with this condition. Patients need to stay informed and work closely with their healthcare providers to explore the most up-to-date treatment options.




