Decoding the Differences: IBD vs IBS
Understanding the differences between Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS) is crucial for individuals experiencing gastrointestinal symptoms. While both conditions affect the digestive system, they have distinct characteristics and require different approaches to diagnosis and treatment.
By clarifying the disparities between IBD and IBS, individuals can seek appropriate medical attention and manage their symptoms effectively. This article aims to provide an in-depth analysis of IBD and IBS, highlighting their unique features and helping readers differentiate between the two.
Understanding IBD and IBS
Definition and Overview of IBD:
Inflammatory Bowel Disease (IBD) refers to a group of chronic inflammatory disorders that primarily affect the gastrointestinal tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. These conditions involve inflammation of the digestive tract, causing symptoms such as abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue. IBD is characterized by periods of flare-ups and remission, and it can lead to long-term complications if left untreated.
Definition and Overview of IBS:
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder that affects the large intestine. Unlike IBD, IBS does not involve inflammation or damage to the digestive tract. Instead, it is characterized by a combination of symptoms, including abdominal pain, bloating, gas, and changes in bowel habits. IBS is a chronic condition, but it does not cause permanent damage to the intestines or increase the risk of colorectal cancer.
Key Differences between IBD and IBS:
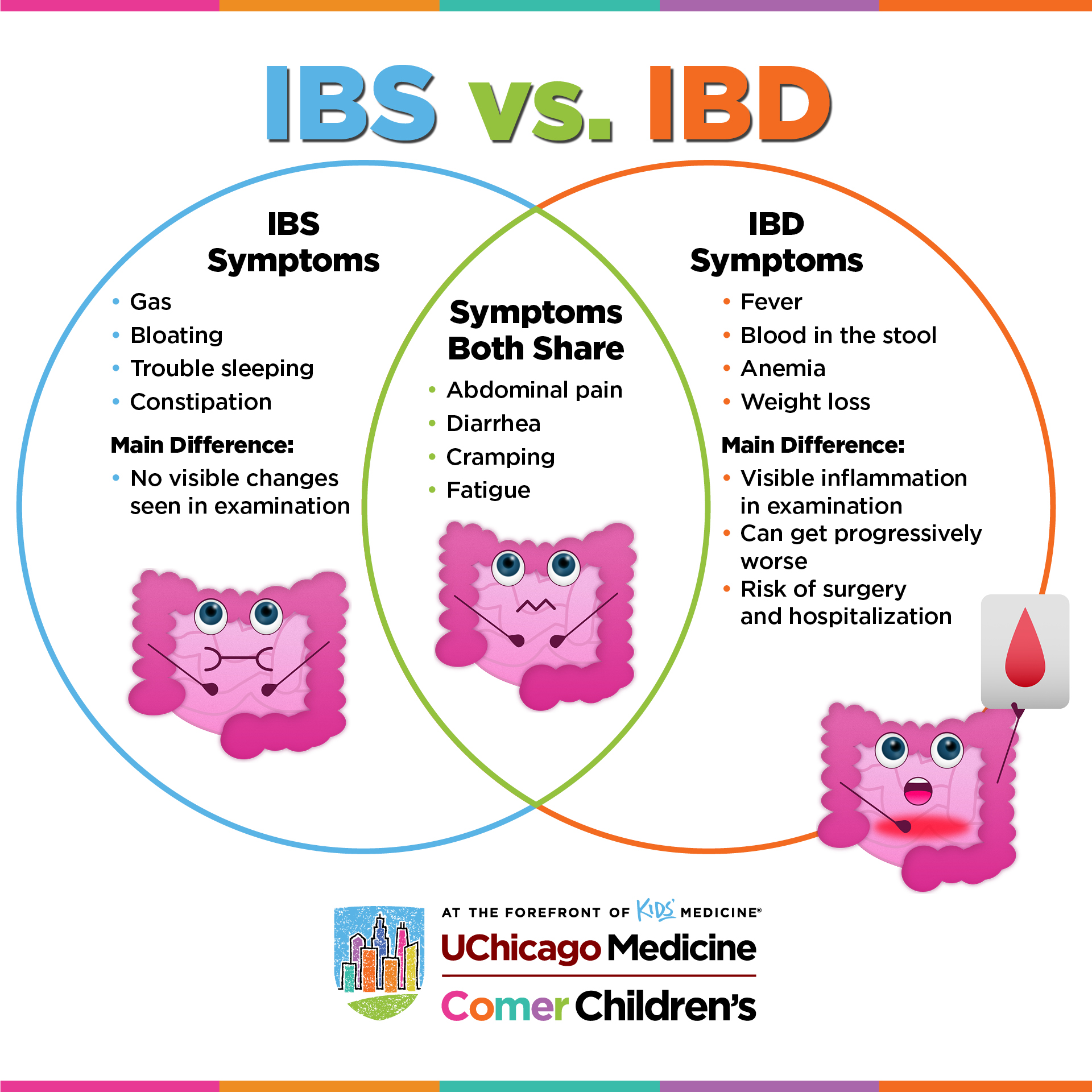
While both IBD and IBS share some similar symptoms, the key distinction lies in the presence of inflammation and structural damage in IBD, which is absent in IBS. Additionally, IBD is considered an autoimmune condition, whereas IBS is a functional disorder. Understanding these fundamental differences is crucial for accurate diagnosis and appropriate treatment.
Differentiating Symptoms
Understanding the specific symptoms associated with IBD and IBS can help individuals distinguish between the two conditions.
Symptoms of IBD
IBD is characterized by a range of symptoms that can vary in severity and location depending on the type and location of the inflammation within the digestive tract. Common symptoms of IBD include:
Abdominal pain and cramping
Diarrhea, often with blood or mucus
Weight loss and reduced appetite
Fatigue and weakness
Fever
Anemia
Rectal bleeding
Joint pain and inflammation
It’s important to note that individuals with IBD may experience periods of remission where their symptoms improve or disappear, followed by flare-ups where symptoms worsen.
Symptoms of IBS
IBS symptoms can vary widely between individuals and may change over time. Common symptoms of IBS include:
Abdominal pain and cramping
Bloating and excessive gas
Diarrhea constipation, or a combination of both
Changes in bowel habits
Mucus in the stool
The feeling of incomplete bowel movements
Unlike IBD, IBS symptoms do not include rectal bleeding, weight loss, or signs of inflammation.
Distinct Symptom Patterns
While IBD and IBS share some similar symptoms, there are distinct patterns that can help differentiate between the two. IBD symptoms often include rectal bleeding, significant weight loss, and signs of inflammation such as fever and joint pain. On the other hand, IBS symptoms primarily revolve around abdominal pain, bloating, and changes in bowel habits without the presence of rectal bleeding or significant weight loss. Understanding these symptom patterns can guide healthcare professionals in making an accurate diagnosis.
Causes and Risk Factors
Exploring the causes and potential triggers of IBD and IBS can provide further insight into the differences between the two conditions.
Causes and Triggers of IBD
The exact cause of IBD is not yet fully understood, but it is believed to result from a combination of genetic, environmental, and immune system factors. Potential triggers and risk factors for IBD include:
Genetic predisposition: Individuals with a family history of IBD are at a higher risk of developing the condition.
Abnormal immune response: The immune system may mistakenly attack the digestive tract, leading to inflammation.
Environmental factors: Certain environmental factors, such as smoking, diet, and exposure to certain infections, may play a role in triggering or exacerbating IBD.
Gut microbiome imbalance: Disruptions in the balance of gut bacteria may contribute to the development of IBD.
Causes and Triggers of IBS
The exact cause of IBS remains unknown, but several factors are believed to contribute to its development. These include:
Abnormalities in the gastrointestinal tract: Individuals with IBS may have a more sensitive or reactive gut, leading to increased pain and discomfort.
Changes in gut motility: Altered movement of the intestines can result in symptoms such as diarrhea or constipation.
Intestinal inflammation: Low-grade inflammation in the intestines may contribute to IBS symptoms.
Psychological factors: Stress, anxiety, and other psychological factors can worsen IBS symptoms.
Dietary triggers: Certain foods and drinks, such as fatty foods, caffeine, and alcohol, may trigger or worsen symptoms in some individuals.
Contrasting Risk Factors
While there may be some overlap, there are distinct risk factors associated with IBD and IBS:
Risk factors for IBD:
Family history of IBD
Smoking
Age (most commonly diagnosed in young adults)
Ethnicity (higher incidence in Caucasians and Ashkenazi Jews)
Risk factors for IBS:
Female gender (more common in women)
Younger age (often begins in late teens or early adulthood)
History of mental health disorders, such as anxiety or depression
History of physical or sexual abuse
Diagnostic Approaches
Accurate diagnosis is essential for differentiating between IBD and IBS. Healthcare professionals employ specific diagnostic approaches for each condition.
Diagnostic Procedures for IBD
Diagnosing IBD typically involves a combination of the following procedures:
Medical history and physical examination: Healthcare professionals will review symptoms, and medical history, and perform a physical examination.
Endoscopy and colonoscopy: These procedures involve the insertion of a flexible tube with a camera into the digestive tract to visualize and assess the extent of inflammation.
Biopsy: During endoscopy or colonoscopy, small tissue samples may be taken for examination under a microscope to confirm the presence of inflammation.
Imaging tests: X-rays, CT scans, or MRI scans may be used to evaluate the digestive tract and identify any complications.
Blood tests: Blood tests can help determine inflammation levels and rule out other potential causes of symptoms.
Diagnostic Procedures for IBS
Diagnosing IBS is primarily based on symptom assessment and the exclusion of other conditions. The following approaches are commonly used:
Medical history and symptom evaluation: Healthcare professionals will review symptoms, and medical history, and assess the presence of specific diagnostic criteria.
Physical examination: A physical examination may be conducted to rule out other potential causes of symptoms.
Diagnostic criteria: Healthcare professionals may refer to established diagnostic criteria, such as the Rome IV criteria, which outline specific symptom patterns and duration required for an IBS diagnosis.
Additional tests: In some cases, healthcare professionals may order additional tests, such as blood tests, stool tests, or imaging studies, to rule out other conditions and provide further reassurance.
Differences in Diagnostic Approaches
The diagnostic approaches for IBD and IBS differ primarily in the use of invasive procedures and the emphasis on ruling out other conditions. IBD diagnosis often involves endoscopy, colonoscopy, and biopsy to visualize and confirm the presence of inflammation. In contrast, IBS diagnosis relies more on symptom assessment and the exclusion of other gastrointestinal disorders. Understanding these differences can help individuals understand the diagnostic process and seek appropriate medical attention.
Treatment Options
Effective management of IBD and IBS involves a multidimensional approach that addresses symptoms, reduces inflammation (in the case of IBD), and improves overall quality of life.
Treatment Options for IBD
The treatment options for IBD aim to reduce inflammation, control symptoms, and prevent complications. These may include:
Medications: Anti-inflammatory drugs, immunosuppressants, biologics, and symptom-specific medications may be prescribed to manage inflammation and alleviate symptoms.
Dietary modifications: Some individuals with IBD may benefit from dietary changes, such as avoiding trigger foods or following a low-residue or low-FODMAP diet.
Lifestyle modifications: Stress management techniques, regular exercise, and adequate sleep can help reduce symptoms and improve overall well-being.
Surgery: In severe cases of IBD, surgery may be necessary to remove damaged portions of the digestive tract or create an ostomy.
Supportive therapies: Counseling, support groups, and complementary therapies like acupuncture or yoga can provide emotional support and help manage stress.
Treatment Options for IBS
The treatment options for IBS focus on symptom management and improving overall gut health. These may include:
Lifestyle modifications: Dietary changes, such as increasing fiber intake, avoiding trigger foods, and eating regular meals, can help alleviate symptoms.
Medications: Over-the-counter or prescription medications, such as antispasmodics, laxatives, or anti-diarrheal drugs, may be used to manage specific symptoms.
Stress management: Stress reduction techniques, such as relaxation exercises, meditation, or cognitive-behavioral therapy, can help manage stress-related symptoms.
Probiotics: Certain strains of probiotics may help improve gut health and alleviate symptoms in some individuals with IBS.
Complementary therapies: Acupuncture, hypnotherapy, or herbal remedies may provide relief for some individuals, but further research is needed to establish their effectiveness.
Contrasting Treatment Approaches
The treatment approaches for IBD and IBS differ primarily due to the presence or absence of inflammation and structural damage. IBD treatment focuses on reducing inflammation, often requiring medication and, in some cases, surgery. IBS treatment, on the other hand, primarily focuses on symptom management through dietary and lifestyle modifications, stress reduction, and targeted medications for symptom relief. Understanding these distinctions is crucial for individuals to receive appropriate treatment and achieve symptom control.
Complications and Prognosis
Both IBD and IBS can have long-term implications on an individual’s health and well-being. Understanding the potential complications and long-term prognosis is important for individuals and healthcare professionals alike.
Potential Complications of IBD
Untreated or poorly managed IBD can lead to various complications, including:
Bowel obstructions: Inflammation and scarring can cause blockages in the intestines, leading to severe pain and potentially requiring surgery.
Malnutrition: Chronic inflammation and reduced nutrient absorption can lead to malnutrition and deficiencies in essential vitamins and minerals.
Perforation or abscesses: Severe inflammation can cause the intestinal walls to weaken, leading to perforations or the formation of abscesses.
Colon cancer: Individuals with long-standing ulcerative colitis have an increased risk of developing colon cancer, requiring regular monitoring and surveillance.
Extraintestinal complications: IBD can also affect other parts of the body, leading to complications such as joint inflammation, skin disorders, and liver problems.
Potential Complications of IBS
IBS itself does not cause structural damage or increase the risk of serious complications. However, it can significantly impact an individual’s quality of life and may lead to the following complications:
Reduced quality of life: Chronic symptoms and unpredictable bowel habits can affect daily activities, work productivity, and social interactions.
Psychological effects: The chronic nature of IBS can lead to anxiety, depression, and increased stress levels.
Increased healthcare utilization: Frequent doctor visits, diagnostic tests, and medication use can contribute to increased healthcare costs.
Impaired social functioning: The need for frequent bathroom breaks and the fear of symptoms can limit social engagements and travel opportunities.
Comparing the Long-term Prognosis
The long-term prognosis of IBD and IBS differs due to the nature of the conditions. IBD is a chronic, progressive condition that requires ongoing management to control inflammation and prevent complications. With appropriate treatment and adherence to medical advice, individuals with IBD can achieve periods of remission and lead relatively normal lives. However, the disease course can be unpredictable, and long-term monitoring is necessary to manage symptoms and prevent complications.
On the other hand, IBS is a functional disorder that does not cause permanent damage to the intestines or increase the risk of serious health complications. While symptoms can be chronic and recurrent, they can often be managed through lifestyle modifications and targeted treatments. With proper self-care and symptom management strategies, individuals with IBS can experience significant improvement in their quality of life.
Lifestyle Management and Support
In addition to medical treatments, lifestyle modifications, and support play a crucial role in managing both IBD and IBS.
Lifestyle Modifications for IBD
Individuals with IBD can benefit from the following lifestyle modifications:
Dietary changes: Working with a registered dietitian can help identify trigger foods and develop an individualized diet plan that supports gut health and minimizes symptoms.
Stress management: Stress reduction techniques, such as mindfulness meditation, deep breathing exercises, and regular physical activity, can help manage stress and potentially reduce flare-ups.
Regular exercise: Engaging in regular physical activity can help improve overall well-being, reduce inflammation, and support healthy digestion.
Adequate sleep: Prioritizing sufficient sleep can help regulate the immune system, reduce inflammation, and support overall health.
Smoking cessation: Quitting smoking is essential for individuals with IBD, as smoking can worsen symptoms and increase the risk of complications.
Lifestyle Modifications for IBS
Lifestyle modifications that can help manage IBS symptoms include:
Identifying trigger foods: Keeping a food diary and eliminating or limiting foods that trigger symptoms can help alleviate discomfort.
Eating regular meals: Establishing a regular eating pattern and avoiding large meals can help regulate bowel movements and reduce symptoms.
Incorporating fiber: Gradually increasing fiber intake from fruits, vegetables, and whole grains can help regulate bowel movements and alleviate constipation.
Stress reduction techniques: Engaging in stress management techniques, such as deep breathing exercises, yoga, or meditation, can help reduce symptom severity.
Regular physical activity: Engaging in regular exercise can improve digestion, reduce stress, and promote overall well-being.
Addressing Support Needs
Both IBD and IBS can have a significant impact on an individual’s emotional well-being. Seeking support from healthcare professionals, support groups, and loved ones can provide valuable assistance in managing the conditions. Support groups specifically tailored for individuals with IBD or IBS can offer a sense of community, shared experiences, and practical tips for coping with symptoms. Additionally, counseling or therapy can help individuals develop coping strategies, manage stress, and address any psychological effects associated with these conditions.
Frequently Asked Questions (FAQs)
What is the main difference between IBD and IBS?
The main difference between IBD and IBS lies in the presence of inflammation and structural damage in IBD, while IBS is a functional disorder without inflammation or damage to the intestines.
Can IBD lead to IBS or vice versa?</strong
No, IBD does not lead to IBS or vice versa. While both conditions can coexist in some individuals, they are distinct entities with different underlying causes and mechanisms.
Are there any specific dietary recommendations for IBD and IBS?
Dietary recommendations for IBD and IBS may vary depending on individual symptoms and triggers. Working with a registered dietitian can help develop personalized dietary plans that cater to specific needs and minimize symptom exacerbation.
How can stress impact IBD and IBS symptoms?
Stress can worsen symptoms in both IBD and IBS. It can trigger flare-ups, increase pain perception, and disrupt normal gut function. Implementing stress management techniques, such as relaxation exercises and mindfulness, can help alleviate symptoms.
Are there any natural remedies that can help with IBD or IBS?
While some individuals may find relief from certain natural remedies, it is important to consult with a healthcare professional before trying any alternative treatments. Natural remedies such as herbal supplements, probiotics, or acupuncture may have varying levels of evidence supporting their efficacy in managing symptoms.
Can IBD or IBS be cured completely?
Currently, there is no known cure for IBD or IBS. However, with appropriate management strategies, including medication, lifestyle modifications, and ongoing medical care, individuals can achieve symptom control and lead fulfilling lives.
Is it possible to have both IBD and IBS simultaneously?
While it is rare, individuals can have both IBD and IBS simultaneously. This can make diagnosis and management more complex, requiring a comprehensive approach that addresses both conditions.
Can pregnancy affect IBD or IBS symptoms?
Pregnancy can have varying effects on IBD and IBS symptoms. Some individuals may experience improvement in symptoms during pregnancy, while others may experience exacerbation. Pregnant individuals with IBD or IBS need to work closely with their healthcare team to manage symptoms and ensure a healthy pregnancy.
What are the potential complications of untreated IBD or IBS?
Untreated or poorly managed IBD can lead to complications such as bowel obstructions, malnutrition, perforation or abscesses, and an increased risk of colon cancer. While IBS does not cause structural damage, untreated or unmanaged symptoms can significantly impact an individual’s quality of life and psychological well-being.
How can I find a support group for individuals with IBD or IBS?
There are various resources available to find support groups for individuals with IBD or IBS. Healthcare professionals, patient advocacy organizations, and online communities can provide information and connect individuals with relevant support groups.
Conclusion
Understanding the differences between IBD and IBS is essential for accurate diagnosis, appropriate treatment, and effective symptom management. While both conditions can cause gastrointestinal symptoms, they have distinct characteristics, including the presence of inflammation and structural damage in IBD. Seeking professional medical advice is crucial for accurate diagnosis and personalized treatment plans. By working closely with healthcare professionals and implementing lifestyle modifications, individuals with IBD or IBS can achieve better symptom control and improve their overall quality of life.
Remember, this article provides general information and should not substitute professional medical advice. If you suspect you may have IBD or IBS, consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.




