Unlocking the Mystery of Parsonage-Turner Syndrome: Understanding the Causes, Symptoms, and Treatment Options
What is Parsonage-Turner Syndrome?
Parsonage Turner Syndrome (PTS), also known as neuralgic amyotrophy, is a condition that affects the nervous system. It is characterized by sudden and severe shoulder pain, followed by weakness and muscle atrophy in the affected area. The exact cause of PTS is still unknown, but it is believed to be related to genetic and environmental factors.
Causes and Risk Factors
The causes of Parsonage-Turner Syndrome are not fully understood, but researchers believe that both genetic and environmental factors play a role. There may be a genetic predisposition to developing the syndrome, as it can sometimes run in families. Environmental factors, such as viral or bacterial infections, trauma, or physical exertion, may trigger the onset of PTS in susceptible individuals.
Several risk factors have been identified for Parsonage-Turner Syndrome. It is more commonly seen in adults between the ages of 20 and 60, with men being slightly more affected than women. Certain medical conditions, such as diabetes and autoimmune disorders, may also increase the risk of developing PTS.
Prevalence and Demographics
Parsonage-Turner Syndrome is a relatively rare condition, with a global prevalence estimated to be around 1 in 100,000 individuals. It can affect people of all ages, but it is most commonly seen in adults. The syndrome has been reported in both males and females, although males tend to be slightly more affected.
Symptoms and Diagnosis
Common Symptoms of Parsonage-Turner Syndrome
Parsonage-Turner Syndrome presents with a range of symptoms that can vary from person to person. The most common symptom is sudden and severe shoulder pain, often described as a sharp or burning sensation. This pain typically occurs on one side of the body and may radiate down the arm.
Following the onset of shoulder pain, weakness and muscle atrophy may develop in the affected area. This can lead to difficulty with arm and shoulder movements, such as lifting objects or reaching overhead. Sensory changes, such as numbness or tingling, may also be experienced.
It is important to note that the symptoms of Parsonage-Turner Syndrome can appear suddenly and progress rapidly, but they can also resolve spontaneously over time. The duration and severity of symptoms can vary widely between individuals.
Differential Diagnosis
Diagnosing Parsonage-Turner Syndrome can be challenging due to its similarity to other conditions that affect the nerves in the shoulder and arm. It is often misdiagnosed as brachial plexus neuropathy or cervical radiculopathy.
Brachial plexus neuropathy is a condition that affects the network of nerves that control the muscles of the shoulder, arm, and hand. Cervical radiculopathy, on the other hand, involves the compression or irritation of nerve roots in the neck region. Both conditions share similarities in symptoms with Parsonage-Turner Syndrome, making it crucial for healthcare professionals to carefully evaluate the patient’s history, physical examination findings, and diagnostic test results to make an accurate diagnosis.
Diagnostic Procedures and Tests
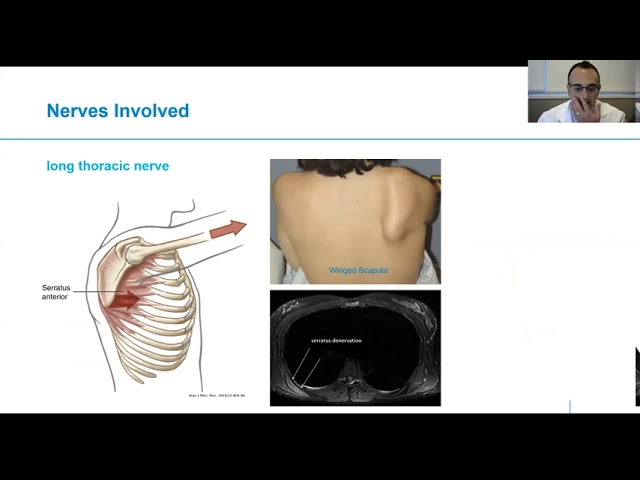
Diagnosing Parsonage-Turner Syndrome involves a combination of clinical assessments, imaging techniques, and electromyography (EMG) tests.
During the clinical assessment, the healthcare provider will evaluate the patient’s medical history and perform a thorough physical examination. They will look for specific signs, such as muscle weakness, atrophy, and sensory changes, that are characteristic of Parsonage-Turner Syndrome.
Imaging techniques, such as magnetic resonance imaging (MRI) or ultrasound, may be used to visualize the affected area and rule out other potential causes of the symptoms. These imaging tests can help identify any structural abnormalities or inflammation in the nerves or surrounding tissues.
Electromyography (EMG) is a specialized test that measures the electrical activity of muscles and the nerves controlling them. It can help determine the extent and severity of nerve damage in Parsonage-Turner Syndrome.
It is important to note that there is no specific test that can definitively diagnose Parsonage-Turner Syndrome. The diagnosis is typically made based on a combination of clinical findings and ruling out other possible causes of the symptoms.
Treatment and Management
Conservative Management Approaches
Treatment for Parsonage-Turner Syndrome often involves a combination of conservative management approaches to alleviate pain, promote healing, and restore function. These approaches may include:
Physical therapy:
A physical therapist can design a customized exercise program to help improve the range of motion, strength, and flexibility in the affected shoulder and arm. They may also use techniques such as manual therapy and modalities like heat or ice to reduce pain and inflammation.
Pain management:
Over-the-counter pain relievers or nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to manage pain and reduce inflammation. In some cases, stronger pain medications or corticosteroid injections may be prescribed.
Assistive devices:
The use of supportive devices, such as slings or braces, can help stabilize the shoulder and provide additional support during daily activities.
Surgical Interventions
In severe cases of Parsonage Turner Syndrome where conservative measures are ineffective or if there is significant nerve damage, surgical intervention may be considered. The specific surgical options will depend on the individual’s condition and the extent of nerve involvement. Some possible surgical interventions include:
Nerve decompression:
This procedure involves relieving pressure on the affected nerves by removing any compressive structures, such as scar tissue or bone spurs.
Nerve transfer:
In cases of severe nerve damage or complete loss of function, a nerve transfer procedure may be performed. This involves transferring a healthy nerve from another part of the body to restore function in the affected area.
Rehabilitation and Recovery
Rehabilitation plays a crucial role in the recovery process for individuals with Parsonage-Turner Syndrome. A tailored exercise program designed by a physical therapist can help restore strength, flexibility, and function in the affected shoulder and arm.
The rehabilitation process may involve a gradual progression of exercises, starting with gentle range of motion movements and gradually incorporating resistance training. The physical therapist will closely monitor the individual’s progress and make adjustments to the program as needed.
Frequently Asked Questions (FAQs)
Q: Can Parsonage-Turner Syndrome be cured?
A: Parsonage-Turner Syndrome cannot be cured, but the symptoms can improve over time with appropriate treatment and management. The recovery process varies from person to person, and some individuals may experience complete resolution of symptoms while others may have residual weakness or limitations.
Q: How long does it take to recover from Parsonage-Turner Syndrome?
A: The recovery time for Parsonage-Turner Syndrome can vary widely. Some individuals may experience improvement in symptoms within a few months, while others may take several years to recover. Early intervention, proper treatment, and adherence to a rehabilitation program can help facilitate the recovery process.
Q: Can Parsonage-Turner Syndrome recur?
A: Parsonage-Turner Syndrome can recur, although it is relatively uncommon. Recurrence may happen in the same or different areas of the body. It is important for individuals who have experienced Parsonage-Turner Syndrome to be aware of potential triggers and seek medical attention if they notice similar symptoms reoccurring.
Q: Is Parsonage-Turner Syndrome hereditary?
A: Parsonage-Turner Syndrome may have a genetic component, as it can sometimes run in families. However, the exact genetic factors involved in the development of the syndrome are still not fully understood. Not everyone with a family history of Parsonage-Turner Syndrome will necessarily develop the condition.
Q: Can physical therapy help with Parsonage-Turner Syndrome?
A: Yes, physical therapy can be beneficial in the management of Parsonage-Turner Syndrome. A physical therapist can design a customized exercise program to improve the range of motion, strength, and function of the affected shoulder and arm. They can also provide guidance on pain management techniques and assistive devices to support recovery.
Q: Are there any lifestyle modifications that can help with Parsonage-Turner Syndrome?
A: Making certain lifestyle modifications can help individuals with Parsonage-Turner Syndrome manage their symptoms and support their recovery. This may include avoiding activities that exacerbate pain or strain the affected area, maintaining good posture, and practicing stress management techniques. It is important to consult with a healthcare professional for personalized advice.
Q: Can Parsonage-Turner Syndrome affect both shoulders?
A: While Parsonage-Turner Syndrome typically affects one shoulder, it is possible for it to occur in both shoulders, although it is relatively rare. Each case of Parsonage-Turner Syndrome is unique, and the symptoms and severity can vary between individuals.
Q: Can Parsonage-Turner Syndrome be prevented?
A: It is not currently possible to prevent Parsonage-Turner Syndrome, as the exact cause of the condition is still unknown. However, managing underlying health conditions, maintaining a healthy lifestyle, and avoiding excessive strain or trauma to the shoulders may help reduce the risk of developing PTS or minimize the severity of symptoms.
Conclusion:
Parsonage-Turner Syndrome, also known as neuralgic amyotrophy, is a condition that affects the nervous system and can cause sudden and severe shoulder pain, weakness, and muscle atrophy. While the exact cause of PTS is still unknown, it is believed to involve a combination of genetic and environmental factors.




