The Thoracentesis Procedure: A Comprehensive Guide to a Life-Saving Intervention
The thoracentesis procedure is a life-saving intervention used to diagnose and treat respiratory conditions. This comprehensive guide aims to provide medical professionals with a thorough understanding of the procedure, its indications, techniques, and potential risks. By enhancing their knowledge and skills in thoracentesis, healthcare providers can ensure safe and effective patient care.
Thoracentesis
What is Thoracentesis?
Thoracentesis is a medical procedure performed to remove fluid or air from the pleural space, the area between the lungs and the chest wall. It is commonly used to diagnose and treat respiratory conditions such as pleural effusion, pneumothorax, and hemothorax. By draining excess fluid or air, thoracentesis helps relieve symptoms, improve breathing, and facilitate further diagnostic investigations.
The Anatomy of the Thoracic Cavity
Understanding the anatomy of the thoracic cavity is crucial for performing a successful thoracentesis. The thoracic cavity is enclosed by the rib cage and contains vital organs such as the lungs, heart, and major blood vessels. Familiarity with the location and structure of these organs helps healthcare providers accurately identify the pleural space and avoid potential complications during the procedure.
Indications for Thoracentesis
Thoracentesis is indicated in various respiratory conditions, including pleural effusion, pneumothorax, hemothorax, and empyema. Common symptoms that may necessitate the procedure include shortness of breath, chest pain, cough, and decreased lung sounds. Diagnostic criteria, such as imaging findings and laboratory tests, help determine the need for thoracentesis and guide further management.
Contraindications and Precautions
While thoracentesis is generally a safe procedure, there are certain contraindications and precautions to consider. Contraindications include patients with uncontrolled bleeding disorders, severe respiratory distress, or infection at the puncture site. Precautions should be taken in patients with significant lung adhesions, uncooperative patients, or those with a small amount of fluid that may be difficult to access. It is important to carefully evaluate each patient’s medical history and condition before proceeding with thoracentesis to minimize potential risks.
Benefits and Risks
Thoracentesis offers several benefits for patients with respiratory conditions. By removing excess fluid or air from the pleural space, it can alleviate symptoms such as difficulty breathing, chest pain, and cough. Additionally, thoracentesis allows for the collection of fluid samples for laboratory analysis, aiding in the diagnosis of underlying conditions. Despite its benefits, thoracentesis carries some risks, including infection, bleeding, lung injury, and pneumothorax. However, these complications are relatively rare, and healthcare providers take precautions to minimize their occurrence.
The Thoracentesis Procedure
Patient Preparation
Prior to performing thoracentesis, it is essential to obtain informed consent from the patient and provide a detailed explanation of the procedure. Patients should be informed about the potential risks, benefits, and alternatives. Pre-procedure tests, such as chest X-rays or ultrasound, may be necessary to assess the location and amount of fluid. Additionally, baseline vital signs and oxygen saturation levels should be obtained to monitor the patient’s condition during the procedure.
Equipment and Sterilization
Several pieces of equipment are required for a successful thoracentesis procedure. These include a sterile thoracentesis tray, a local anesthetic, a thoracentesis needle, a syringe, and collection containers for fluid samples. It is crucial to maintain a sterile environment throughout the procedure to minimize the risk of infection. All equipment should be properly sterilized, and healthcare providers should follow strict aseptic techniques to prevent contamination.
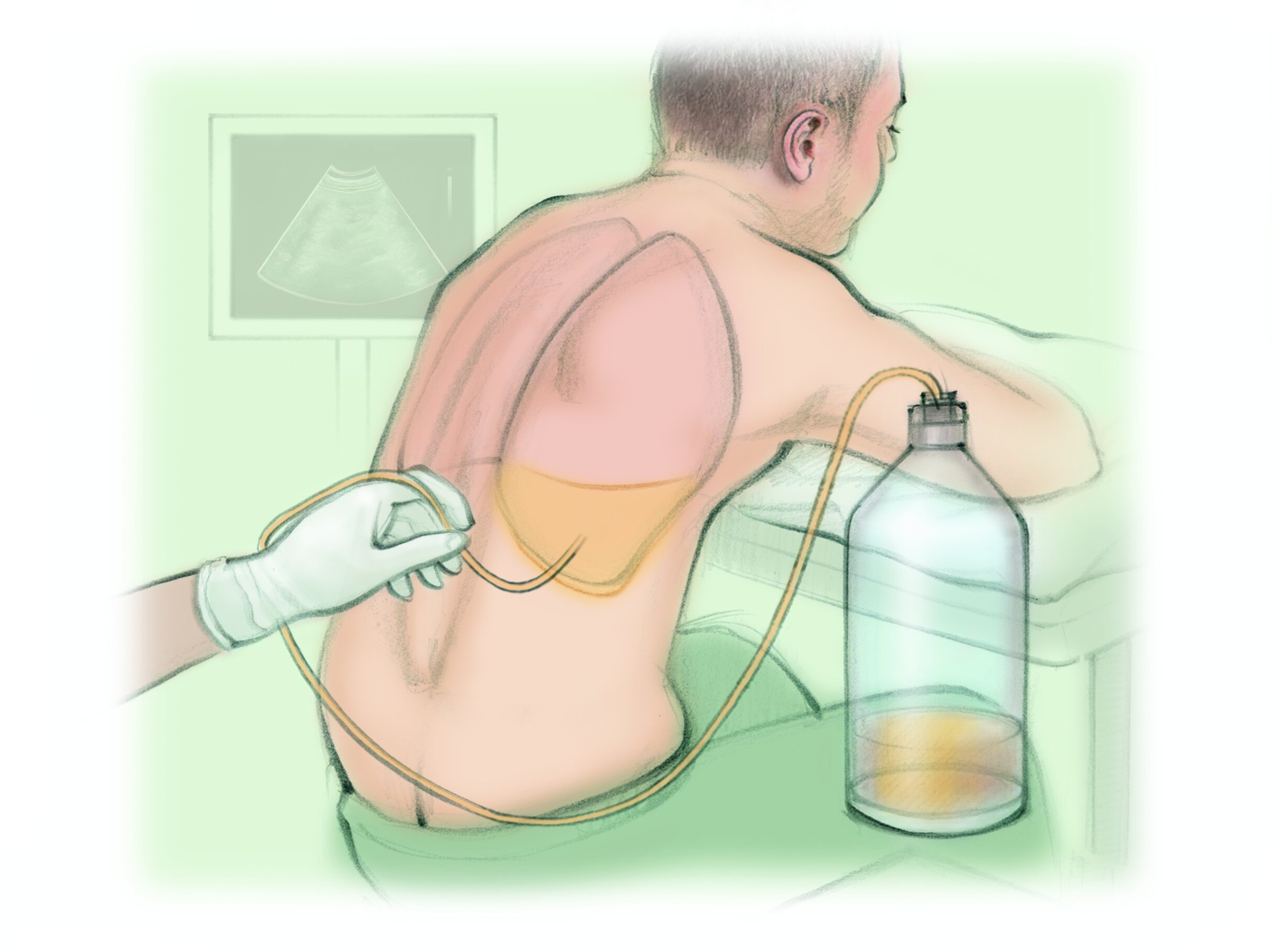
Positioning the Patient
The positioning of the patient plays a crucial role in the success and safety of thoracentesis. The patient should be seated upright or positioned on their side with the affected side facing upwards. This positioning helps to maximize access to the pleural space and allows for better visualization during the procedure. It is important to ensure the patient’s comfort and safety throughout the process, providing adequate support and reassurance.
Anesthesia and Analgesia
To minimize pain and discomfort during thoracentesis, various anesthesia options can be utilized. Local anesthesia, such as lidocaine, is commonly administered to numb the skin and underlying tissues at the puncture site. This helps reduce pain during needle insertion. In some cases, conscious sedation may be considered to help alleviate anxiety and provide additional pain relief. The choice of anesthesia depends on the patient’s condition, preferences, and the healthcare provider’s judgment.
The Thoracentesis Technique
The thoracentesis procedure involves several steps to ensure safe and effective fluid or air removal. After proper anesthesia, a needle is inserted through the skin and into the pleural space under ultrasound or fluoroscopic guidance. Once the needle is in place, fluid or air is aspirated using a syringe, and the collected samples are carefully labeled for further analysis. Throughout the procedure, healthcare providers should closely monitor the patient’s vital signs and response to ensure a successful outcome.
Collection and Analysis of Fluid
The collected fluid samples should be handled with care to maintain their integrity for laboratory analysis. Each sample should be properly labeled with the patient’s information, the date and time of collection, and the site from which it was obtained. The samples are then sent to the laboratory for analysis, which may include cell counts, biochemical analysis, microbiological cultures, and cytology. The results of these tests help in diagnosing the underlying condition and guiding further treatment decisions.
Post-Procedure Care and Follow-up
After thoracentesis, it is important to closely monitor the patient for any potential complications or adverse reactions. Vital signs should be regularly assessed, and the puncture site should be inspected for signs of infection or bleeding. Patients may be advised to avoid strenuous activities for a certain period and to report any worsening symptoms or new onset complications. Follow-up appointments should be scheduled to evaluate the patient’s progress and determine theneed for further interventions or treatments.
Frequently Asked Questions (FAQs)
What are the common risks associated with thoracentesis?
The common risks associated with thoracentesis include infection, bleeding, lung injury, and pneumothorax. However, these complications are relatively rare and can be minimized by following proper sterile techniques, using ultrasound guidance, and carefully monitoring the patient during and after the procedure.
How long does the thoracentesis procedure usually take?
The duration of the thoracentesis procedure can vary depending on factors such as the amount of fluid or air to be removed and the patient’s condition. On average, the procedure takes about 15 to 30 minutes. However, it is important to allocate sufficient time for patient preparation, anesthesia administration, and post-procedure care.
Is thoracentesis a painful procedure?
Thoracentesis is typically performed under local anesthesia, which helps numb the puncture site and minimize pain. Some patients may experience mild discomfort or pressure during the procedure, but it is generally well-tolerated. Healthcare providers may also offer additional pain relief measures, such as conscious sedation, for patients who are particularly anxious or sensitive to pain.
Are there any alternatives to thoracentesis?
In certain cases, alternative interventions may be considered instead of thoracentesis. These alternatives include chest tube placement, pleurodesis, or surgical interventions such as video-assisted thoracoscopic surgery (VATS). The choice of intervention depends on the underlying condition, the patient’s overall health, and the recommendations of the healthcare team.
Can thoracentesis be performed on pregnant patients?
Thoracentesis can be performed on pregnant patients, but caution should be exercised due to the potential risks to both the mother and the fetus. The procedure should be carefully evaluated and discussed with the patient, taking into consideration the potential benefits and risks. Close monitoring of the patient’s condition and fetal well-being is essential throughout the procedure.
What should I expect after the thoracentesis procedure?
After the thoracentesis procedure, patients may experience mild soreness or discomfort at the puncture site. Some patients may notice a decrease in their symptoms, such as improved breathing. It is important to follow any post-procedure instructions provided by the healthcare team, including restrictions on activities and any prescribed medications. If there are any concerns or worsening symptoms, it is crucial to contact the healthcare provider for further evaluation.
How frequently can thoracentesis be performed on a patient?
The frequency of thoracentesis depends on the individual patient’s condition and the underlying cause of the fluid or air accumulation. In some cases, a single thoracentesis procedure may be sufficient to alleviate symptoms and resolve the underlying issue. However, in certain chronic conditions, such as recurrent pleural effusions, multiple thoracentesis procedures or alternative interventions may be required over time. The healthcare team will determine the appropriate frequency based on the patient’s needs.
Can complications arise after the thoracentesis procedure?
While complications after thoracentesis are relatively rare, they can occur. Delayed complications may include infection, bleeding, subcutaneous emphysema, or persistent air leaks. It is important for patients to be aware of the signs and symptoms of these complications and to seek immediate medical attention if they arise. Regular follow-up appointments with the healthcare provider can help monitor for any potential complications.
What are the possible outcomes of a thoracentesis procedure?
The outcomes of a thoracentesis procedure can vary depending on the underlying condition being treated. In many cases, thoracentesis provides symptom relief, improves lung function, and aids in the diagnosis of the underlying cause. However, the long-term prognosis and outcomes depend on the specific condition and the overall health of the patient. It is important to discuss the expected outcomes with the healthcare provider based on the individual case.
Are there any special considerations for pediatric patients?
Performing thoracentesis on pediatric patients requires special considerations due to their smaller size and unique physiological factors. Pediatric patients may require sedation or general anesthesia to ensure their comfort and cooperation during the procedure. Careful monitoring and coordination with pediatric specialists are essential to ensure the safety and well-being of these young patients.
Conclusion
Thoracentesis is a life-saving procedure used to diagnose and treat respiratory conditions. By understanding the procedure, its




