Thrombosis vs. Embolism: Understanding the Critical Differences
Cardiovascular health is a topic of paramount importance, and within this vast domain, two terms often surface thrombosis and embolism. Understanding the differences between these two conditions is crucial because they pertain to blood clots, which can have serious consequences. In this comprehensive guide, we delve into the intricate realm of thrombosis vs. embolism, shedding light on their definitions, causes, symptoms, and treatments. Armed with this knowledge, you can become a proactive guardian of your cardiovascular well-being.
What Is Thrombosis?
Definition:
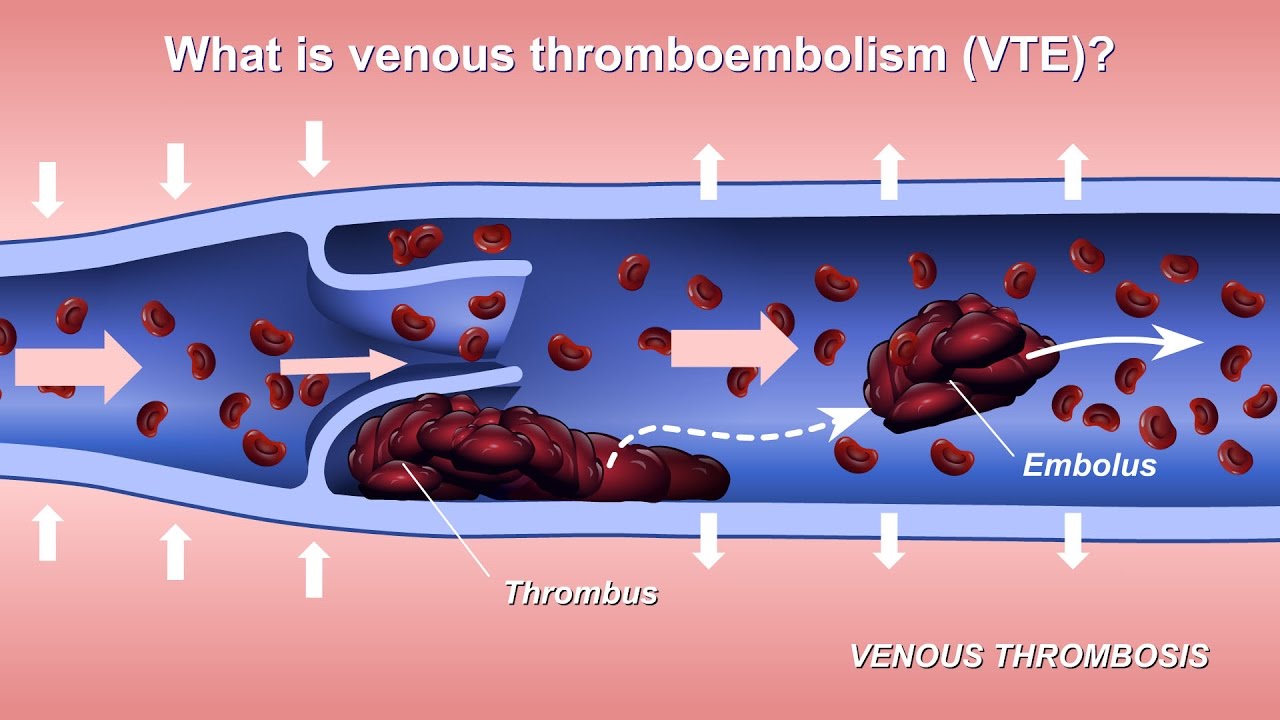
Thrombosis refers to the formation of blood clots, known as thrombi, within blood vessels. These clots can obstruct the flow of blood and potentially lead to a host of health issues.
Causes:
Thrombosis can occur for various reasons, often attributed to an imbalance in the coagulation (clotting) process. Common causes include prolonged immobility, surgery, genetic predisposition, and certain medical conditions like deep vein thrombosis (DVT).
Symptoms:
Thrombosis manifests with symptoms such as localized pain, swelling, warmth, and redness in the affected area. If a clot breaks free and travels through the bloodstream, it can result in a more serious condition called embolism.
Treatment:
Timely intervention is crucial. Treatment typically involves blood-thinning medications (anticoagulants) to prevent the clot from enlarging and to reduce the risk of new clots forming. In some cases, more invasive measures like clot-dissolving medications (thrombolytics) or surgical procedures may be necessary.
What Is Embolism?
Definition:
Embolism is the movement of a blood clot (embolus) from its site of origin to another part of the body through the bloodstream. This clot can obstruct blood vessels, leading to potentially life-threatening situations.
Causes:
The source of emboli (plural of embolus) can vary. They may originate from thrombi within the veins or arteries, or they can be composed of other substances like fat globules, air bubbles, or even foreign objects introduced during medical procedures.
Symptoms:
The symptoms of embolism largely depend on the location where the embolus becomes lodged. Common signs include sudden shortness of breath, chest pain, rapid pulse, and in some cases, altered mental state if the embolus affects the brain.
Treatment:
Immediate medical attention is imperative in cases of suspected embolism. Treatment may involve medications to dissolve the clot (thrombolytics) or interventions like thrombectomy (surgical removal of the clot) in critical situations. Preventive measures to avoid embolism are crucial, particularly for individuals at higher risk.
Thrombosis vs. Embolism: Key Differences
Now that we’ve established definitions and causes, let’s delve into the critical differences between thrombosis and embolism. Understanding these distinctions is pivotal in recognizing the symptoms and seeking appropriate medical care when needed.
Risk Factors for Embolism:
Thrombosis:
A history of thrombosis increases the risk of embolism, as clots formed during thrombosis can break free and become emboli.
Heart Conditions:
Certain heart conditions, like atrial fibrillation, can create an environment where clots form in the heart and potentially embolize.
Surgery or Medical Procedures:
Some medical procedures can introduce air bubbles or debris into the bloodstream, increasing the risk of embolism.
Atherosclerosis:
Hardening and narrowing of the arteries (atherosclerosis) can lead to the formation of clots that may embolize.
Preventive Measures for Embolism:
Anticoagulants:
For individuals at a high risk of embolism due to medical conditions or surgeries, anticoagulant medications may be prescribed as a preventive measure.
Managing Underlying Conditions:
Effectively managing heart conditions, atherosclerosis, and other underlying health issues can reduce the risk of clot formation.
Prophylactic Procedures:
In some cases, healthcare providers may use filters or other measures to prevent emboli from traveling to critical organs.
Thrombosis vs. Embolism: The Role of Knowledge
Being informed about thrombosis and embolism, their risk factors, and potential symptoms is the first step in prevention. Recognizing when to seek medical help can be life-saving. Additionally, knowing your risk factors, especially if you have a family history or underlying medical conditions, empowers you to make informed decisions about your health.
Risk Factors for Thrombosis:
Prolonged Immobility:
Extended periods of immobility, such as long flights or bed rest after surgery, increase the risk of DVT.
Inherited Conditions:
Some individuals may have genetic predispositions that make them more susceptible to clot formation.
Medical Conditions:
Conditions like cancer, heart disease, and inflammatory disorders can elevate the risk of thrombosis.
Medications:
Certain medications, such as hormonal birth control or hormone replacement therapy, may increase clotting risk.
Preventive Measures for Thrombosis:
Stay Active:
Regular physical activity, including walking and leg exercises during long flights or bed rest, can help maintain healthy blood flow.
Hydration:
Adequate hydration supports blood circulation, reducing the risk of clot formation.
Compression Stockings:
If at risk, wearing compression stockings can help prevent DVT during extended immobility.
Medication:
In some cases, healthcare providers may prescribe anticoagulant medications as a preventive measure, especially for individuals with a high risk of thrombosis due to medical conditions or surgeries.
Risk Factors for Embolism:
Thrombosis:
A history of thrombosis increases the risk of embolism, as clots formed during thrombosis can break free and become emboli.
Heart Conditions:
Certain heart conditions, like atrial fibrillation, can create an environment where clots form in the heart and potentially embolize.
Surgery or Medical Procedures:
Some medical procedures can introduce air bubbles or debris into the bloodstream, increasing the risk of embolism.
Atherosclerosis:
Hardening and narrowing of the arteries (atherosclerosis) can lead to the formation of clots that may embolize.
Preventive Measures for Embolism:
Anticoagulants:
For individuals at a high risk of embolism due to medical conditions or surgeries, anticoagulant medications may be prescribed as a preventive measure.
Managing Underlying Conditions:
Effectively managing heart conditions, atherosclerosis, and other underlying health issues can reduce the risk of clot formation.
Prophylactic Procedures:
In some cases, healthcare providers may use filters or other measures to prevent emboli from traveling to critical organs.
Thrombosis vs. Embolism: The Role of Knowledge
Being informed about thrombosis and embolism, their risk factors, and potential symptoms is the first step in prevention. Recognizing when to seek medical help can be life-saving. Additionally, knowing your risk factors
Diagnosis and Medical Evaluation
When it comes to thrombosis and embolism, timely and accurate diagnosis is of utmost importance. Healthcare providers use various tools and tests to determine the presence of clots and assess their potential impact. Let’s explore these diagnostic procedures:
Ultrasound Imaging:
This non-invasive imaging technique, known as Doppler ultrasound, is often the first choice for diagnosing DVT. It uses sound waves to create images of blood flow in the veins, revealing the presence of clots.
D-Dimer Test:
This blood test measures the presence of a substance called D-dimer, which is often elevated in the presence of an abnormal blood clot. However, a positive D-dimer result doesn’t confirm a clot; further imaging is usually required.
CT Pulmonary Angiography:
In cases of suspected pulmonary embolism (PE), a CT pulmonary angiography is a valuable tool. It involves injecting a contrast dye into a vein and using a CT scanner to visualize the pulmonary arteries.
Treatment Approaches
Treatment for thrombosis and embolism aims to prevent the clot from growing larger, breaking apart, or recurring, and to reduce the risk of complications. The specific treatment plan depends on the location, size, and severity of the clot. Let’s explore the main treatment approaches:
Anticoagulant Medications:
Also known as blood thinners, these medications are commonly prescribed for both thrombosis and embolism. They prevent existing clots from enlarging and reduce the risk of new clots forming. Common anticoagulants include heparin and warfarin, as well as newer oral anticoagulants like rivaroxaban and apixaban.
Thrombolytic Therapy:
In cases of severe or extensive clotting, healthcare providers may use thrombolytic medications to dissolve the clot rapidly. This approach is more invasive and typically reserved for critical situations.
Real-Life Impact: Stories and Awareness
Real-life stories and experiences can provide valuable insights into the challenges and consequences of thrombosis and embolism. These conditions can affect people of all ages and backgrounds, highlighting the importance of awareness and proactive healthcare. In the next section, we will share some real-life cases and experiences to shed light on the impact of these conditions.
Frequently Asked Questions (FAQs) about Thrombosis and Embolism
1. What is thrombosis?
Thrombosis is the formation of a blood clot, or thrombus, within a blood vessel. It can occur in veins (venous thrombosis) or arteries (arterial thrombosis).
2. What is embolism?
Embolism refers to the condition where a clot or other material, known as an embolus, travels through the bloodstream and lodges in a blood vessel, obstructing blood flow.
3. What are the common risk factors for thrombosis?
Common risk factors for thrombosis include prolonged immobility, inherited conditions, medical conditions like cancer and heart disease, and certain medications.
4. How is deep vein thrombosis (DVT) diagnosed?
DVT is often diagnosed using ultrasound imaging, which creates images of blood flow in the veins. The D-dimer blood test may also be used, followed by imaging confirmation.
5. What are the symptoms of pulmonary embolism (PE)?
PE symptoms can include sudden shortness of breath, chest pain, rapid heart rate, and coughing up blood. Severe cases may lead to fainting or shock.
6. Can embolism occur without a prior thrombosis (clot) formation?
Yes, embolism can occur without a prior thrombosis. Other materials like air bubbles or debris can also cause embolism.
7. How are blood clots treated?
Treatment options for blood clots include anticoagulant medications (blood thinners), thrombolytic therapy to dissolve clots, surgical thrombectomy, and vena cava filters.
8. Are there preventive measures for thrombosis and embolism during long flights?
Yes, during long flights, staying active by moving your legs, staying hydrated, and wearing compression stockings can help prevent DVT.
9. What is the role of genetics in thrombosis risk?
Genetic factors can increase the risk of thrombosis. Some individuals may have genetic conditions that make them more prone to clot formation.
10. Can thrombosis and embolism be prevented?
Prevention strategies include staying active, managing underlying medical conditions, taking prescribed medications, and using prophylactic measures in high-risk situations.
Conclusion:
Knowledge is a powerful tool when it comes to thrombosis and embolism. Understanding the risk factors, recognizing symptoms, and knowing when to seek medical help can save lives. Whether you’re a healthcare professional, a patient, or simply someone interested in maintaining good health, staying informed about these conditions is a crucial step toward better cardiovascular well-being.




