The Mysteries of Vasomotor Symptoms: A Comprehensive Guide
Understanding Vasomotor Symptoms
What are Vasomotor Symptoms?
Vasomotor symptoms (VMS) refer to a range of physical sensations experienced by individuals, often characterized by sudden and intense feelings of heat, flushing, and excessive sweating. These symptoms are commonly known as hot flashes, night sweats, and flushes.
Causes and Triggers of Vasomotor Symptoms
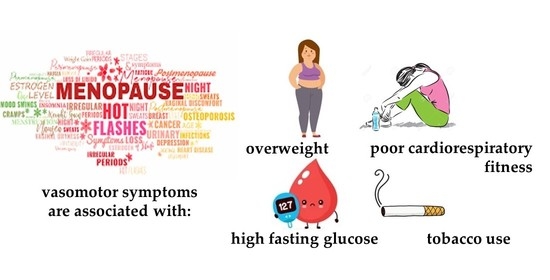
Vasomotor symptoms can be triggered by hormonal changes, particularly during menopause, perimenopause, and postmenopause. Fluctuations in estrogen and progesterone levels affect the body’s thermoregulation, leading to VMS. Additionally, certain medications, medical conditions, and lifestyle factors can also contribute to the occurrence of VMS.
Mechanisms Behind Vasomotor Symptoms
Vasomotor symptoms are primarily influenced by the hypothalamus, a part of the brain responsible for regulating body temperature. Hormonal fluctuations during menopause disrupt the hypothalamus’s thermoregulatory function, causing the sudden onset of hot flashes and other VMS. These symptoms are a result of the body’s attempt to cool down and restore temperature balance.
Symptom Management and Treatment Options
Lifestyle Modifications
Making certain lifestyle modifications can help manage vasomotor symptoms effectively. Firstly, paying attention to dietary choices by avoiding triggers such as spicy foods and caffeine can reduce the frequency and intensity of VMS. Incorporating foods rich in phytoestrogens, such as soy products and flaxseeds, may also provide relief. Additionally, practicing temperature regulation techniques like layering clothing, using fans or cooling devices, and keeping the bedroom cool can help alleviate symptoms.
Non-Hormonal Therapies
Non-hormonal therapies are available for individuals who prefer alternatives to hormone replacement therapy (HRT). Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), gabapentin, and clonidine are commonly prescribed medications that can help reduce the frequency and severity of VMS. It is important to discuss the benefits, potential side effects, and considerations of each option with a healthcare professional to determine the most suitable choice.
Hormonal Therapies
Hormone replacement therapy (HRT) is an effective treatment option for managing vasomotor symptoms, particularly in women experiencing menopause. HRT involves the use of estrogen and, in some cases, progesterone to replace the hormones that decline during menopause. It can be administered orally, through transdermal patches, or vaginally. However, it is essential to consider the potential risks and benefits associated with HRT, as it may have certain side effects and is not suitable for everyone. Consulting a healthcare professional is crucial in determining the appropriate course of action.
Frequently Asked Questions (FAQs)
What is the average duration of vasomotor symptoms?
The average duration of vasomotor symptoms can vary from person to person. In general, these symptoms can last for a few months to several years. However, it’s important to note that some individuals may experience VMS for a shorter or longer duration. Consulting a healthcare professional can provide a better understanding of individual circumstances.
Can vasomotor symptoms occur in men?
While vasomotor symptoms are commonly associated with menopause in women, men can also experience them. In men, VMS can occur due to hormonal imbalances, certain medical conditions, or as a side effect of certain medications. It is essential for men experiencing VMS to consult a healthcare professional for proper evaluation and guidance.
Are vasomotor symptoms always related to menopause?
No, vasomotor symptoms are not always related to menopause. While menopause is a common cause of VMS in women, these symptoms can also occur due to other factors such as hormonal fluctuations during perimenopause, postmenopause, or even in women who have undergone surgical removal of the ovaries. Additionally, certain medications, medical conditions (such as thyroid disorders), and lifestyle factors (such as stress and obesity) can contribute to the occurrence of vasomotor symptoms. It is important to consult with a healthcare professional to determine the underlying cause of VMS and develop an appropriate management plan.
Can lifestyle changes alone effectively manage vasomotor symptoms?
Lifestyle changes can play a significant role in managing vasomotor symptoms. Simple modifications in diet and daily habits can help alleviate the frequency and intensity of VMS. Avoiding triggers such as spicy foods, caffeine, and alcohol, as well as maintaining a healthy weight through regular exercise can have a positive impact. Temperature regulation techniques, such as dressing in layers and using fans or cooling devices, can also provide relief. However, it is important to note that lifestyle changes may not eliminate vasomotor symptoms for everyone. In cases where symptoms persist or significantly affect daily life, medical interventions such as hormone therapy or non-hormonal treatments may be necessary. Consulting a healthcare professional can help determine the most effective approach for individual symptom management.
Are there any natural remedies for vasomotor symptoms?
Some individuals may seek natural remedies to manage vasomotor symptoms. While scientific evidence is limited, certain herbal remedies such as black cohosh, evening primrose oil, and red clover have been suggested to provide relief. Additionally, practices like acupuncture, mindfulness-based stress reduction, and yoga have shown some potential benefits. However, it is important to exercise caution when using natural remedies and consult with a healthcare professional, as the effectiveness and safety of these options can vary. They may also interact with other medications or have contraindications for certain individuals.
What are the risks associated with hormone replacement therapy?
Hormone replacement therapy (HRT) carries certain risks that need to be considered before starting treatment. Estrogen-only HRT may increase the risk of endometrial cancer in women who have not undergone a hysterectomy. However, combining estrogen with progesterone in women with a uterus can help reduce this risk. Other potential risks associated with HRT include an increased risk of blood clots, stroke, heart disease, and breast cancer. The risks and benefits of HRT should be carefully evaluated on an individual basis, taking into account personal medical history and risk factors. Regular monitoring and follow-up with a healthcare professional are essential for maintaining the appropriate balance between symptom management and potential risks.
Can vasomotor symptoms be a sign of a more serious health condition?
In most cases, vasomotor symptoms are a natural part of the hormonal changes occurring during menopause or other related conditions. However, in some instances, VMS can be a sign of an underlying medical condition. Certain thyroid disorders, such as hyperthyroidism, can cause symptoms similar to hot flashes. It is important to consult with a healthcare professional if vasomotor symptoms are accompanied by other concerning symptoms, persist for an extended period, or significantly impact daily life. A thorough evaluation can help determine the underlying cause and ensure appropriate management.
Conclusion:
Vasomotor symptoms can be challenging to manage, but with the right understanding and approach, individuals can find relief and improve their quality of life. By comprehending the causes, triggers, and mechanisms behind VMS, as well as exploring various treatment options, including lifestyle modifications, non-hormonal therapies, and hormone replacement therapy, individuals can make informed decisions in consultation with healthcare professionals. Additionally, addressing frequently asked questions and dispelling common misconceptions can provide clarity and guidance to those experiencing vasomotor symptoms. Ongoing research and advancements in this field continue to expand our knowledge and may lead to further breakthroughs in the management of these symptoms.




