Exploring Wound Vac Therapy: Benefits, Process, and Uses
Wound vac therapy, also known as negative pressure wound therapy (NPWT), has revolutionized wound healing by offering an innovative approach to managing complex wounds. In this comprehensive guide, we’ll delve into the fundamentals of wound vac therapy, shedding light on its uses, benefits, and the intricate process that fuels its effectiveness. Whether you’re a healthcare professional seeking insights or an individual exploring wound treatment options, this article aims to provide you with a thorough understanding of this transformative therapy.
When Is Wound Vac Therapy Recommended?
Wound vac therapy isn’t a one-size-fits-all solution; rather, it serves as a powerful tool in the management of specific wounds. Healthcare providers often recommend wound vac therapy for a range of scenarios, including acute and chronic wounds, surgical incisions, and non-healing ulcers. These wounds may arise from surgical procedures, traumatic injuries, diabetic foot ulcers, pressure sores, and more. By tailoring the therapy to different wound types, wound vac therapy aims to accelerate healing and improve patient outcomes.
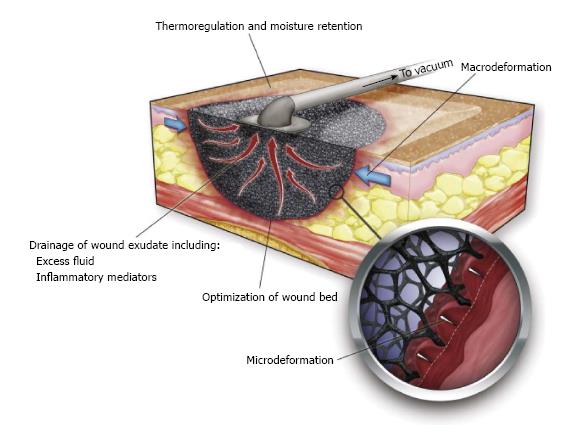
How Does Wound Vac Therapy Work?
At the heart of wound vac therapy is the concept of negative pressure. This therapy involves the application of controlled, sub-atmospheric pressure to the wound area, creating a sealed environment with a specialized dressing. The vacuum pump connected to the dressing removes excess fluids, promoting the removal of bacteria, promoting blood flow, and encouraging the formation of granulation tissue—a key factor in wound healing. This innovative approach addresses multiple aspects of wound healing simultaneously, ultimately leading to faster and more effective recovery.
Understanding the Components of a Wound Vac System
A wound vac system comprises several essential components that work in tandem to facilitate the healing process. The heart of the system is the vacuum pump, which generates negative pressure and regulates it according to the wound’s needs. This pump is connected to a drainage tubing, which is attached to a specialized wound dressing applied to the wound site. The dressing creates a seal that ensures a controlled environment for the negative pressure to take effect. Together, these components create an environment that supports wound healing by promoting circulation, reducing swelling, and facilitating the removal of excess fluid and debris.
Benefits of Wound Vac Therapy for Wound Healing
Wound vac therapy offers a plethora of benefits that make it a preferred choice for wound management. By enhancing blood flow to the wound site, the therapy accelerates the formation of granulation tissue—the foundation of new skin. The controlled environment created by the wound vac system reduces edema, minimizes infection risk, and aids in removing harmful substances from the wound. Additionally, wound vac therapy can reduce the need for frequent dressing changes, thereby enhancing patient comfort and reducing the risk of disturbing the wound healing process.
The Wound Vac Process: Step-by-Step Overview
The wound vac process involves several key steps, each contributing to its effectiveness. First, the wound is cleaned and a specialized wound dressing is applied. The vacuum pump is connected to the dressing, initiating the negative pressure. This pressure removes excess fluid, stimulates blood flow, and encourages tissue growth. Over time, as the wound heals, the negative pressure may be adjusted. Dressing changes occur at regular intervals, during which the wound is cleaned, and a new dressing is applied. Throughout the process, healthcare professionals closely monitor progress, making adjustments as needed.
Potential Candidates for Wound Vac Therapy
Wound vac therapy is a versatile treatment option suitable for various types of wounds and conditions. Individuals who may benefit from this therapy include those with surgical wounds, diabetic ulcers, pressure sores, traumatic injuries, and open wounds that are challenging to heal. Moreover, patients with wounds that exhibit signs of slow healing or are at risk of infection can also find relief through wound vac therapy. Healthcare providers assess the wound’s characteristics, size, location, and overall health status to determine if wound vac therapy is the appropriate choice.
Expected Outcomes and Considerations
The effectiveness of wound vac therapy is evidenced by its ability to promote quicker wound healing and improved outcomes. Patients undergoing this therapy often experience reduced wound size, increased tissue formation, and a decrease in wound-related pain. However, it’s essential to note that individual responses can vary. Factors such as the patient’s overall health, wound severity, and adherence to therapy instructions play a role in determining outcomes. A collaborative approach between patients and healthcare professionals is crucial for achieving the best possible results.
Limitations and Possible Complications
While wound vac therapy offers numerous benefits, it’s essential to be aware of its limitations and potential complications. Some wounds may not be suitable for this therapy, such as those with exposed blood vessels or organs. Additionally, patients with certain medical conditions may require careful evaluation before undergoing wound vac therapy. Possible complications include skin irritation or breakdown at the dressing site, discomfort during dressing changes, and infection risk if not managed properly. Working closely with healthcare professionals minimizes these risks and ensures safe and effective therapy.
Frequently Asked Questions (FAQs)
Q: What is wound vac therapy, and how does it work?
A: Wound vac therapy, or negative pressure wound therapy (NPWT), involves using negative pressure to aid wound healing. It creates an environment that promotes blood flow, reduces swelling, and encourages tissue growth.
Q: Who can benefit from wound vac therapy?
A: Wound vac therapy is beneficial for individuals with various wound types, including surgical wounds, diabetic ulcers, pressure sores, and slow-healing wounds. Healthcare professionals assess the wound’s characteristics to determine suitability.
Q: How does wound vac therapy accelerate wound healing?
A: Wound vac therapy accelerates healing by enhancing blood flow, promoting the formation of granulation tissue, and aiding in the removal of excess fluids and debris from the wound.
Q: Are there different types of wound vac systems?
A: Yes, wound vac systems comprise components like vacuum pumps, drainage tubing, and specialized dressings. Variations in these components cater to different wound sizes and types.
Q: Is wound vac therapy painful?
A: Wound vac therapy is generally well-tolerated. During dressing changes, patients may experience mild discomfort, which can be managed with appropriate pain relief methods.
Q: How long does wound vac therapy usually last?
A: The duration of wound vac therapy varies based on the wound’s severity, size, and individual healing progress. Healthcare providers determine the appropriate treatment duration.
Q: What are the expected outcomes of wound vac therapy?
A: Patients often experience reduced wound size, improved tissue formation, and decreased pain. However, individual responses vary, and outcomes depend on factors like overall health.
Q: Can wound vac therapy be used for all types of wounds?
A: While wound vac therapy is effective for many wounds, certain conditions, such as exposed blood vessels or organs, may not be suitable for this therapy. Healthcare professionals evaluate suitability.
Q: What are the potential complications of wound vac therapy?
A: Possible complications include skin irritation, discomfort during dressing changes, and infection risk if not managed properly. Regular monitoring and communication with healthcare providers mitigate these risks.
Q: How can I ensure the success of wound vac therapy?
A: Success relies on collaboration between patients and healthcare professionals. Adhering to therapy instructions, attending regular appointments, and promptly addressing concerns contribute to optimal results.
Conclusion: Empowering Wound Healing
Wound vac therapy stands as a beacon of hope for individuals dealing with complex wounds that require specialized care. By delving into the intricacies of wound vac therapy, its benefits, process, and considerations, this article aimed to provide you with a comprehensive understanding. Whether you’re a patient seeking effective wound management or a healthcare professional exploring treatment options, the knowledge gained here equips you to make informed decisions and embark on a healing journey optimized for success. Remember, open communication with healthcare providers and a proactive approach are key to harnessing the transformative power of wound vac therapy for enhanced wound healing.




