Hypopneas: Unveiling the Hidden Sleep Disorder
In the realm of sleep disorders, hypopneas often linger in the shadows, yet their impact on our well-being is profound. In this comprehensive guide, we embark on a journey to unravel the mysteries of hypopneas, shedding light on what they are, their causes, and the critical need for understanding them. Join us as we explore how hypopneas can disrupt your sleep and health, and discover the steps to manage them effectively.
What Are Hypopneas?
Demystifying Hypopneas: Breathing Troubles in the Night
Before delving into the complexities of hypopneas, let’s start with the basics. Hypopneas are episodes of shallow or abnormally slow breathing during sleep. Unlike their more notorious cousin, sleep apnea, where breathing pauses completely, hypopneas involve partial airflow restriction. This distinction may seem subtle, but it has significant implications for your sleep quality and overall health.
Causes of Hypopneas
Uncovering the Culprits: What Leads to Hypopneas?
Understanding the root causes of hypopneas is essential to address the issue effectively. Several factors can contribute to the occurrence of hypopneas, and recognizing them is the first step toward improving your sleep quality. Let’s explore the common triggers behind these disruptive breathing patterns.
Common Causes of Hypopneas:
Obesity:
Excess weight can exert pressure on the airway, leading to restricted airflow.
Nasal Congestion:
Allergies or respiratory conditions that cause nasal congestion can increase the risk of hypopneas.
Alcohol and Sedatives:
The relaxation of throat muscles induced by these substances can exacerbate breathing issues during sleep.
Signs and Symptoms
Hypopneas often occur silently, but they leave behind subtle clues that shouldn’t be ignored. If you suspect you or a loved one may be experiencing hypopneas, watch out for these common signs and symptoms:
Interrupted Breathing:
You may notice periods of shallow or slow breathing, often accompanied by gasping or choking sounds.
Loud Snoring:
While not exclusive to hypopneas, persistent and disruptive snoring can be a sign of underlying breathing issues.
Excessive Daytime Fatigue:
Hypopneas disrupts restorative sleep, leading to daytime drowsiness, fatigue, and difficulty concentrating.
Diagnosis and Testing
Identifying hypopneas typically requires a healthcare professional’s expertise and specialized tests. Here’s a glimpse into the diagnostic methods used to confirm the presence of hypopneas and assess their severity:
Diagnostic Methods for Hypopneas:
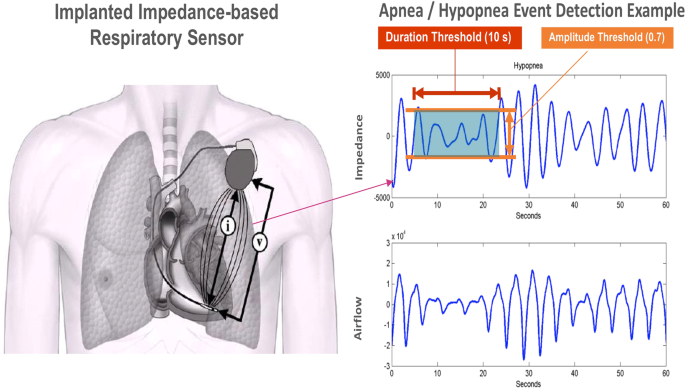
Polysomnography (Sleep Study):
This comprehensive test monitors various body functions during sleep, including airflow, oxygen levels, and brain activity.
Home Sleep Tests:
Some cases may be diagnosed using portable devices that measure essential sleep parameters, such as breathing patterns and oxygen saturation.
Health Implications
Beyond Sleep: The Health Consequences of Untreated Hypopneas
While hypopneas may seem inconspicuous, the impact they have on your health is far-reaching. Untreated hypopneas can lead to a cascade of health problems, and understanding these implications is vital for taking action.
Potential Health Consequences:
Cardiovascular Issues:
Hypopneas strain the heart and increase the risk of conditions like hypertension and heart disease.
Cognitive Impairment:
Poor sleep quality due to hypopneas can impair memory, concentration, and overall cognitive function.
Treatment Options
Managing Hypopneas: Your Path to Better Sleep
Now that we’ve explored the intricacies of hypopneas, it’s time to discuss how they can be effectively managed. Fortunately, several treatment options are available, tailored to your specific needs and circumstances.
Treatment Approaches for Hypopneas:
Lifestyle Changes:
Begin with simple adjustments such as weight loss, positional therapy (changing sleep positions), and avoiding alcohol and sedatives before bedtime.
Continuous Positive Airway Pressure (CPAP) Therapy:
CPAP machines deliver a continuous stream of air to keep your airway open during sleep.
Oral Appliances:
These devices reposition the jaw and tongue to prevent airway obstruction, often recommended for mild to moderate cases.
Lifestyle Changes
Empowering Yourself: Lifestyle Modifications for Hypopneas
Taking proactive steps to address hypopneas often begins with lifestyle changes. These adjustments can significantly improve your sleep quality and reduce the frequency of breathing disruptions.
Lifestyle Modifications for Managing Hypopneas:
Weight Management:
Losing excess weight can alleviate pressure on the airway, reducing the risk of hypopneas.
Sleep Position:
Sleeping on your side instead of your back can prevent airway collapse.
Avoiding Triggers:
Steer clear of alcohol, sedatives, and heavy meals close to bedtime to minimize muscle relaxation in the throat.
CPAP and Oral Appliances
Harnessing Technology: CPAP and Oral Appliances for Hypopneas
For those with moderate to severe hypopneas, technological solutions like CPAP therapy and oral appliances can be game-changers in improving sleep quality and overall well-being.
Understanding CPAP Therapy and Oral Appliances:
Continuous Positive Airway Pressure (CPAP):
A CPAP machine delivers a continuous flow of air through a mask, preventing airway collapse during sleep.
Oral Appliances:
These custom-fitted devices reposition the jaw or tongue to keep the airway open, particularly effective for mild to moderate cases.
Surgical Options
Exploring Surgical Solutions: When All Else Fails
In rare cases where lifestyle changes, CPAP therapy, and oral appliances prove insufficient in managing hypopneas, surgical interventions may be considered. Let’s delve into these surgical options and the circumstances under which they become necessary.
Surgical Interventions for Hypopneas:
Uvulopalatopharyngoplasty (UPPP):
This surgery involves removing excess tissue from the throat to widen the airway.
Genioglossus Advancement (GA):
GA repositions the tongue attachment to prevent airway collapse.
FAQs about Hypopneas: A Comprehensive Guide
Q1: Can hypopneas occur without snoring?
Yes, hypopneas can occur without snoring. While snoring is a common symptom, not everyone with hypopneas snores.
Q2: Are hypopneas the same as sleep apnea?
No, hypopneas and sleep apnea are related but distinct conditions. Hypopneas involve partial airflow restriction, while sleep apnea includes complete pauses in breathing during sleep.
Q3: Can lifestyle changes alone effectively manage hypopneas?
For mild cases, lifestyle changes like weight loss and sleep position adjustments can be effective. However, more severe cases may require additional treatments.
Conclusion
In this comprehensive guide to hypopneas, we’ve shed light on the often-overlooked sleep disorder that can significantly impact your life. From understanding the causes and symptoms to exploring various treatment options, you now possess the knowledge to take action and regain control over your sleep and overall health. Remember, seeking professional guidance is crucial if you suspect you have hypopneas. Restful, uninterrupted sleep is within reach, and this journey begins with knowledge and proactive steps.




