Mastering Open Heart Surgery Recovery: Your Comprehensive Guide
Open heart surgery is a life-saving medical procedure that often marks a turning point in a person’s health journey. While the surgery itself is crucial, what comes after is equally significant—open heart surgery recovery. In this comprehensive guide, we’ll take you through the essential steps and insights for a successful recovery. Whether you’re a patient, a family member, or a caregiver, understanding the process is key to ensuring the best possible outcome.
Understanding Open Heart Surgery
Open heart surgery, also known as cardiac surgery, is a complex procedure performed to correct a variety of heart-related issues. Here, we’ll provide an overview of what open heart surgery entails and why it may be necessary for patients.
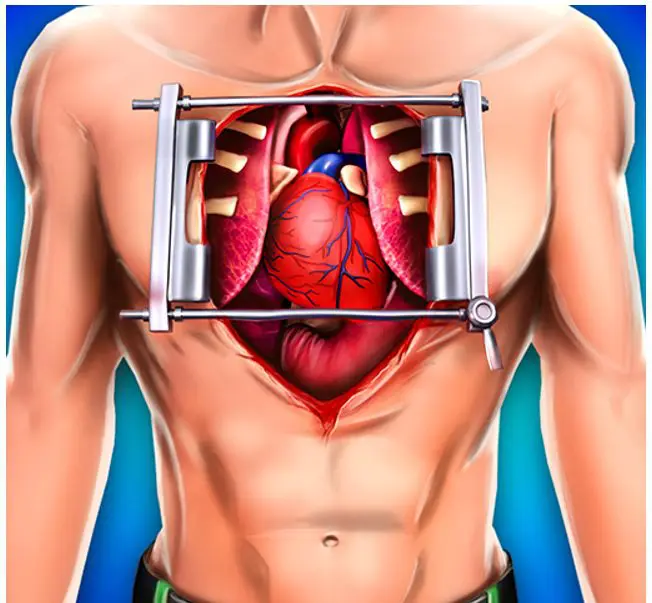
What is Open Heart Surgery?
Open heart surgery is a surgical procedure that involves opening the chest to access the heart. It’s used to treat a range of heart conditions, such as coronary artery disease, valve problems, and congenital heart defects.
Why is Open Heart Surgery Performed?
Patients undergo open heart surgery for several reasons, including repairing or replacing heart valves, bypassing blocked arteries, and correcting structural abnormalities. The goal is to improve heart function and overall health.
Types of Open Heart Surgery
There are different types of open heart surgeries, each targeting specific heart issues. Some of the most common procedures include coronary artery bypass grafting (CABG), heart valve surgery, and congenital heart defect repair.
Preparing for Surgery and Recovery
Preparing for open heart surgery is a crucial phase that can significantly impact the success of the procedure and subsequent recovery. Here, we’ll discuss how patients and their support systems can get ready for this challenging but transformative journey.
Mental and Emotional Preparation
Open heart surgery can be emotionally taxing. Patients need to prepare themselves mentally by seeking support from loved ones, joining support groups, or speaking with a therapist if needed.
Physical Preparation
Physical preparation includes maintaining a healthy lifestyle before surgery, such as managing chronic conditions, quitting smoking, and following a balanced diet. These steps can contribute to better surgical outcomes.
Gathering Support
Patients should build a reliable support network consisting of family members, friends, and caregivers who can assist in the recovery phase. This support system plays a vital role in the overall healing process.
The Open Heart Surgery Procedure
Understanding what happens during open heart surgery is fundamental to comprehending the challenges and expectations of recovery. In this section, we’ll provide an overview of the surgical procedure itself.
The Operating Room
Open heart surgery takes place in a specialized operating room equipped with advanced medical technology and a highly skilled surgical team.
Anesthesia and Incision
The procedure begins with the administration of anesthesia to ensure the patient is asleep and pain-free. Surgeons then make an incision in the chest, typically along the breastbone (sternum).
Cardiopulmonary Bypass
To temporarily take over the heart’s pumping function, a heart-lung machine (cardiopulmonary bypass machine) is used. This allows the surgical team to work on the heart while it’s still.
Repair or Replacement
Depending on the specific reason for surgery, the surgeon will repair or replace heart valves, bypass blocked arteries, or address other cardiac issues.
Closing the Chest
Once the necessary repairs or procedures are completed, the surgeon closes the chest using sutures or wires. A temporary pacemaker may be implanted to regulate the heart’s rhythm during the initial recovery phase.
Immediate Post-Operative Care
The immediate hours and days following open heart surgery are critical. In this section, we’ll discuss what patients can expect during this initial phase of recovery.
Recovery in the Intensive Care Unit (ICU)
After surgery, patients are transferred to the ICU for close monitoring. Medical staff will track vital signs, manage pain, and ensure a stable recovery.
Ventilation and Breathing
Patients may be connected to a ventilator to assist with breathing. Gradually, as they regain strength, the ventilator support is reduced.
Pain Management
Pain control is a priority during this phase. Medications are administered to alleviate discomfort and manage post-operative pain.
Monitoring and Testing
Continuous monitoring includes regular electrocardiograms (ECGs or EKGs), blood tests, and other assessments to check the heart’s function and overall health.
Early Mobility
Encouraging early mobility is essential. Physical therapists may work with patients to initiate gentle movements and exercises while in the ICU.
Early Recovery at the Hospital
As patients progress in their recovery journey, they transition from the intensive care unit (ICU) to a regular hospital room. This section outlines what patients can expect during this phase.
Transition to a Regular Room
Typically, patients move to a regular hospital room when they are stable and no longer require intensive care. It’s a positive sign of progress.
Continued Monitoring
While in a regular room, patients continue to be closely monitored. Medical staff assess vital signs, wound healing, and overall well-being.
Pain Management
Pain management remains a priority. Medications are adjusted as needed to ensure patient comfort while minimizing side effects.
Wound Care
Proper wound care is essential. Patients are instructed on how to care for their surgical incision and are monitored for any signs of infection.
Diet and Nutrition
Nutritional support is vital for healing. Patients may start with a liquid diet and gradually transition to solid foods as tolerated.
Physical Therapy
Physical therapists work with patients to gradually increase mobility and strength. This includes simple exercises and walking.
Going Home and Continuing Recovery
Transitioning from the hospital to home marks a significant milestone in the recovery process. This section guides what patients and caregivers should be prepared for during this transition.
Discharge Planning
Discharge planning begins well in advance. Healthcare providers and case managers collaborate to ensure a smooth transition home.
Medications and Follow-up Care
Patients receive detailed instructions on medication management and upcoming appointments with healthcare providers.
Home Environment
Preparing the home environment for recovery is essential. This may include making adjustments for mobility and ensuring a safe, comfortable space.
Emotional Support
Emotional support remains crucial at home. Family members and caregivers play a vital role in providing reassurance and assistance.
Gradual Resumption of Daily Activities
Patients are encouraged to gradually resume daily activities, such as walking and light household chores, under the guidance of their healthcare team.
Long-Term Recovery and Rehabilitation
The journey of open heart surgery recovery extends beyond the initial hospitalization and home transition. This section explores the importance of long-term recovery and rehabilitation.
Cardiac Rehabilitation Programs
Cardiac rehabilitation programs offer structured exercise, education, and support for heart surgery patients. Participation can enhance recovery and reduce the risk of future heart issues.
Lifestyle Adjustments
Patients are encouraged to make positive lifestyle changes, including adopting a heart-healthy diet, engaging in regular exercise, quitting smoking, and managing stress.
Medication Management
Long-term medication management is often necessary to control blood pressure, cholesterol levels, and other heart-related factors.
Regular Follow-up Visits
Scheduled follow-up visits with healthcare providers are essential to monitor progress and address any emerging issues.
Psychological and Emotional Well-being
The emotional impact of open heart surgery can be significant. Patients should be aware of available resources for managing stress, anxiety, and depression.
Potential Complications and When to Seek Help
While open heart surgery has a high success rate, complications can arise. This section outlines potential complications and when to seek immediate medical attention.
Infection
Surgical site infections can occur. Signs of infection include increased redness, swelling, or discharge from the incision site.
Bleeding
Excessive bleeding should be addressed promptly. It may present as blood soaking through dressings or sudden, severe bruising.
Breathing Problems
Difficulty breathing, chest pain, or persistent coughing should not be ignored. These symptoms may indicate lung issues.
Irregular Heartbeat
Changes in heart rhythm or palpitations should be reported. These can sometimes indicate arrhythmias.
Fever
A persistent fever may signal an underlying infection and should be evaluated by a healthcare provider.
Frequently Asked Questions (FAQs) related to open heart surgery:
Q1: What is open heart surgery?
A: Open heart surgery, also known as cardiac surgery, is a surgical procedure performed on the heart or its major blood vessels. It often involves opening the chest to access the heart.
Q2: Why is open heart surgery performed?
A: Open heart surgery is performed to treat various heart conditions, including coronary artery disease, heart valve problems, congenital heart defects, and aortic aneurysms.
Q3: How long does open heart surgery typically take?
A: The duration of open heart surgery varies depending on the specific procedure and the patient’s condition. It can range from a few hours to several hours.
Q4: What is the recovery time for open heart surgery?
A: The recovery time can vary, but most patients spend about 6 to 8 weeks in the recovery phase. Full recovery may take several months to a year.
Q5: What can I expect during the immediate post-operative phase?
A: After surgery, you’ll be closely monitored in the intensive care unit (ICU). You may be on a ventilator to assist with breathing.
Q6: When can I resume normal daily activities, like driving or working?
A: The timeline for resuming normal activities varies by individual and the type of surgery performed. Driving may be allowed after a few weeks, while returning to work may take longer.
Q7: Are there dietary restrictions during open heart surgery recovery?
A: Yes, you’ll likely follow a heart-healthy diet, which may include restrictions on sodium and saturated fats. Your healthcare team will provide specific dietary guidelines.
Q8: Is it normal to feel emotional during recovery?
A: Yes, it’s common to experience a range of emotions during recovery. This can include anxiety, depression, or stress. Seeking support from loved ones or counseling can help manage these feelings.
Q9: Can I resume exercise and physical activity after open heart surgery?
A: Yes, but it should be done gradually and under the guidance of your healthcare team. Cardiac rehabilitation programs are often recommended to safely reintroduce physical activity.
Q10: What are the signs of a possible infection at the surgical site?
A: Signs of infection can include increased redness, swelling, warmth, or discharge from the incision site. Fever may also indicate an infection and should be reported to your healthcare provider.
Conclusion
In conclusion, open heart surgery recovery is a multifaceted journey that encompasses physical, emotional, and psychological aspects. By understanding the surgical procedure, preparing for recovery, and staying committed to long-term well-being, patients can increase their chances of a successful recovery.




