Peripheral Arterial Disease (PAD) is a serious vascular condition that affects millions of Americans—often without their knowledge. While many may dismiss early symptoms as signs of aging or unrelated health issues, PAD is a progressive disease that can significantly impact your quality of life and increase the risk of severe complications such as heart attack, stroke, or even limb amputation if left untreated.
PAD is more common than most people realize. According to the Society for Vascular Surgery, approximately 8 million people in the U.S. are affected. Alarmingly, nearly 70% of individuals with PAD are undiagnosed, mainly because the symptoms can be subtle or mistaken for other conditions.
What Is Peripheral Arterial Disease (PAD)?
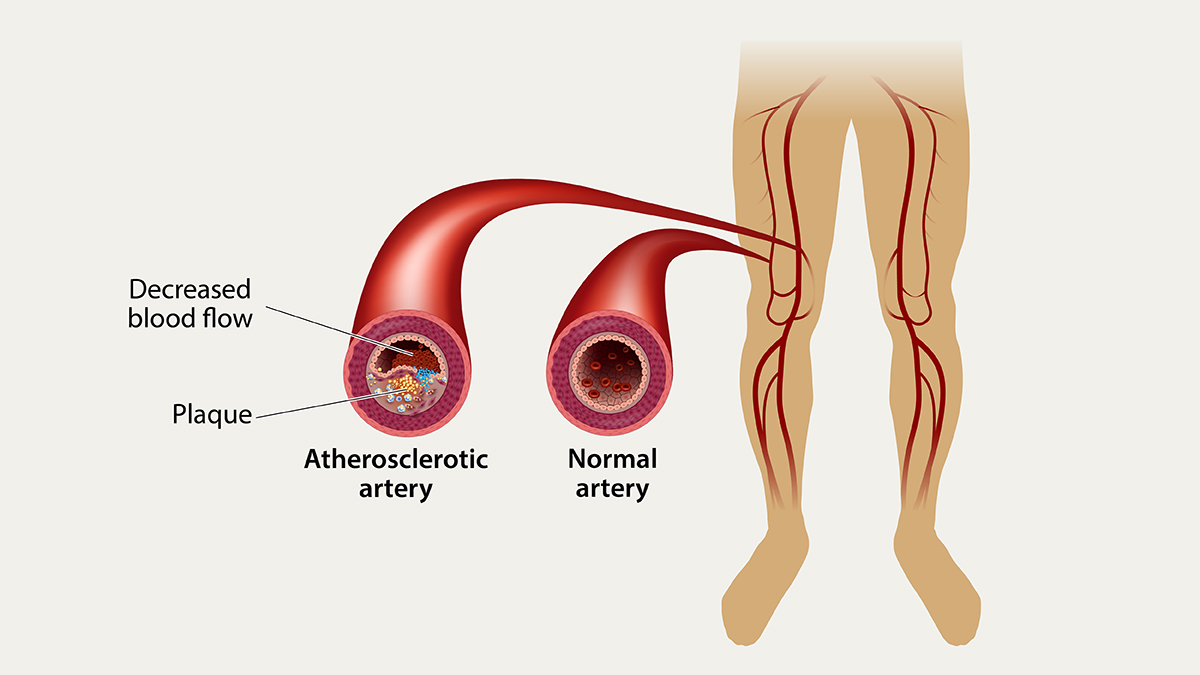
PAD occurs when fatty deposits, or plaque, build up on the walls of arteries that supply blood to your arms and legs. This process, known as atherosclerosis, causes the arteries to narrow or become completely blocked, reducing blood flow. The legs are most commonly affected, leading to pain, mobility issues, and poor wound healing.
PAD vs. PVD: What’s the Difference?
PAD is often confused with Peripheral Vascular Disease (PVD). While PAD specifically refers to arterial blockages, PVD is a broader term that includes conditions affecting all blood vessels outside of the heart and brain, including veins and lymphatic vessels. Understanding this distinction is important for proper diagnosis and treatment.
Recognizing the Symptoms of PAD
The symptoms of PAD can range from mild discomfort to severe complications. Here are the most common signs to look out for:
Common Symptoms:
-
Intermittent leg pain or cramping, especially while walking or climbing stairs (claudication)
-
Numbness or tingling in the legs or feet
-
Sores or wounds on the legs or feet that heal slowly or not at all
-
Coldness in one leg or foot compared to the other
-
Shiny skin or hair loss on the legs
-
Weak or absent pulses in the legs or feet
These symptoms often worsen over time and may become constant, especially at night.
Major Risk Factors for PAD
PAD shares many risk factors with cardiovascular diseases like coronary artery disease and stroke. Understanding these risk factors can help in early detection and prevention.
Modifiable (Changeable) Risk Factors:
-
Smoking – The single most significant preventable risk
-
Diabetes – Poorly controlled blood sugar damages blood vessels
-
High blood pressure – Causes stress on artery walls
-
High cholesterol – Promotes plaque buildup
-
Obesity – Increases overall strain on the vascular system
-
Sedentary lifestyle – Lack of exercise reduces circulation
Non-Modifiable (Unchangeable) Risk Factors:
-
Age (65+) – Risk increases with age
-
Gender (Male) – Men are more likely to develop PAD
-
Family history – Genetic predisposition to vascular disease
-
Race/Ethnicity – African Americans and Hispanics have a higher prevalence
Is Peripheral Arterial Disease Preventable?
Yes—while PAD is a serious condition, many cases are preventable with lifestyle changes and proper medical care. Taking proactive steps before symptoms begin is the best defense against PAD.
How to Lower Your Risk of PAD:
-
Quit smoking and avoid exposure to secondhand smoke
-
Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins
-
Exercise regularly—aim for at least 30 minutes of moderate activity most days
-
Manage chronic conditions like high blood pressure, diabetes, and high cholesterol
-
Take medications as prescribed to prevent blood clots or reduce cholesterol
-
Maintain a healthy weight
-
Limit alcohol consumption
These changes not only reduce your PAD risk but also support overall cardiovascular health.
Importance of Early Diagnosis and Specialized Care
Because PAD symptoms can mimic other conditions—or appear mild in the early stages—many people delay seeking care. This delay can lead to complications like:
-
Non-healing ulcers
-
Infections
-
Gangrene
-
Limb amputation
When to See a Vascular Specialist
If you’re experiencing any of the symptoms listed above—or if you have multiple risk factors—it’s crucial to see a vascular specialist. These experts can perform diagnostic tests like ankle-brachial index (ABI) or ultrasound imaging to assess blood flow in your limbs.
Take Charge of Your Vascular Health
Your primary care physician is the first point of contact in managing PAD risk. They can guide you through lifestyle changes, prescribe medications, and refer you to a specialist when needed.
Early intervention is key. Whether you have mild symptoms or are at risk due to age and lifestyle, don’t wait—proactive care can save limbs and lives.
FAQs
Q1. What is the main cause of PAD?
A: PAD is primarily caused by atherosclerosis, a buildup of fatty plaque in the arteries that restricts blood flow, especially to the legs.
Q2. Can PAD be cured?
A: While there is no cure, PAD can be effectively managed through lifestyle changes, medication, and, in severe cases, surgical interventions like angioplasty.
Q3. Is PAD life-threatening?
A: If untreated, PAD can lead to serious complications such as limb loss, heart attack, and stroke. Early detection and treatment significantly lower the risks.
Q4. How is PAD diagnosed?
A: PAD is diagnosed through tests such as the ankle-brachial index (ABI), Doppler ultrasound, and blood tests to check cholesterol and glucose levels.
Q5. Who should get screened for PAD?
A: Individuals over 65, or over 50 with risk factors like smoking or diabetes, should discuss PAD screening with their doctor.




