Mastering Thoracentesis: Procedure
Thoracentesis, a medical procedure that involves the removal of fluid or air from the space around the lungs, plays a crucial role in diagnosing and treating various respiratory conditions. In this comprehensive guide, we’ll delve into the intricacies of thoracentesis, offering you a clear understanding of what it entails, why it’s necessary, and how it can benefit your health. Whether you’re a healthcare professional or someone curious about medical procedures, this article aims to provide valuable insights into thoracentesis.
Thoracentesis
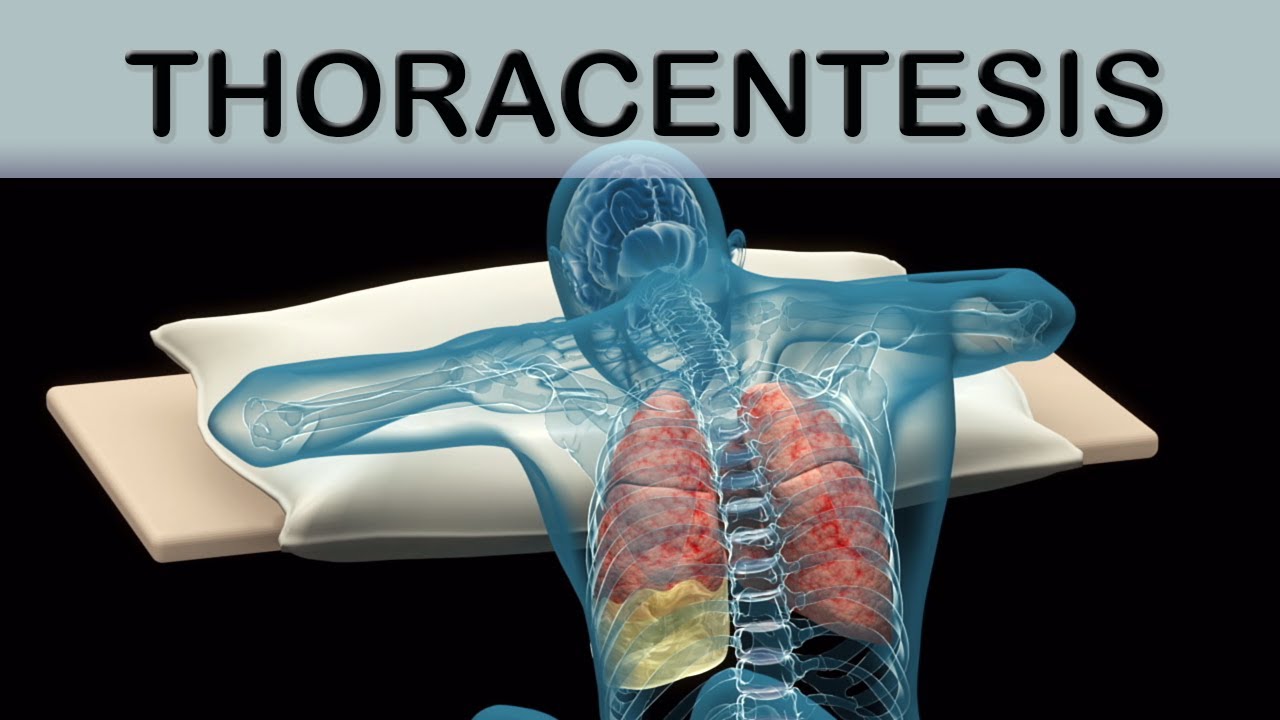
Thoracentesis, often referred to as a pleural tap or chest tap, is a medical procedure used to remove fluid or air that accumulates in the pleural space—the space between the lung and the chest wall. This procedure serves both diagnostic and therapeutic purposes, making it an essential tool in the realm of respiratory medicine.
Indications and Symptoms
To appreciate the significance of thoracentesis, it’s essential to recognize the symptoms and medical conditions that may necessitate this procedure. Some of the common indications include:
Dyspnea (Shortness of Breath):
Individuals experiencing unexplained or severe shortness of breath may undergo thoracentesis to determine its underlying cause.
Chest Pain:
Patients with chest pain, especially when it worsens with deep breathing or coughing, might require thoracentesis to evaluate potential pleural effusion (fluid accumulation).
Respiratory Infections:
In cases of recurrent respiratory infections or pneumonia, thoracentesis can aid in diagnosing and managing the condition effectively.
Cancer Diagnosis:
Thoracentesis may be performed to collect pleural fluid samples for laboratory analysis, helping in the detection and staging of lung cancer or other malignancies.
Pleural Effusion:
The buildup of excess fluid in the pleural space can result from various medical conditions, and thoracentesis is often the go-to procedure for its removal and analysis.
Preparation for Thoracentesis
Preparing for a thoracentesis procedure is essential to ensure a safe and effective experience. Patients should be well-informed about what to expect and how to cooperate with healthcare professionals. Here, we outline the necessary steps for a smooth preparation process.
Medical History and Assessment
Before scheduling a thoracentesis, your healthcare provider will conduct a comprehensive medical evaluation. This assessment includes:
Review your medical history to identify any underlying conditions or medications that may affect the procedure.
Performing a physical examination to assess your overall health and lung function.
Ordering relevant diagnostic tests, such as chest X-rays or CT scans, to visualize the pleural space and pinpoint the fluid or air buildup.
Informed Consent
Informed consent is a crucial step in the preparation process. Your healthcare provider will explain the procedure, its purpose, potential risks, and alternatives. Feel free to ask questions to clarify any concerns. Only proceed with the procedure once you fully understand and consent to it.
Fasting and Medications
In most cases, fasting for a few hours before thoracentesis is recommended. Your healthcare provider will provide specific instructions regarding when to stop eating and drinking. Additionally, you may be asked to temporarily discontinue certain medications, especially blood thinners, to reduce the risk of bleeding during the procedure.
Positioning
During thoracentesis, you’ll typically sit upright on the edge of a bed or examination table, with your arms resting on a bedside table or in your lap. Maintaining a stable and comfortable position is crucial for the procedure’s success.
Local Anesthesia
To minimize discomfort during thoracentesis, your healthcare provider will administer a local anesthetic to numb the area where the needle will be inserted. This step ensures that you feel minimal pain or discomfort during the procedure.
The Thoracentesis Procedure: Step by Step
Thoracentesis is a medical procedure performed by trained healthcare professionals to safely remove excess fluid or air from the pleural space. In this section, we break down the thoracentesis procedure into its steps, providing you with a clear understanding of what happens during this essential diagnostic and therapeutic process.
Positioning and Sterile Preparation
Before the procedure begins, you will be positioned upright, as previously discussed during the preparation phase. The area around the site where the needle will be inserted is thoroughly cleaned and sterilized to minimize the risk of infection.
Local Anesthesia
To ensure your comfort and minimize pain, the healthcare provider will administer a local anesthetic to numb the skin and underlying tissue at the insertion site. This is typically done using a small needle, causing only a brief, mild discomfort.
Needle Insertion
Once the anesthesia takes effect, a thin, hollow needle is carefully inserted through the skin and into the pleural space. This step requires precision to avoid injury to surrounding structures.
Fluid or Air Removal
A syringe or vacuum bottle connected to the needle is used to gently withdraw the excess fluid or air. The healthcare provider carefully monitors the entire process to ensure safety and efficiency.
Sample Collection
If thoracentesis is being performed for diagnostic purposes, a portion of the removed fluid may be sent to a laboratory for analysis. This analysis helps identify the underlying cause of pleural effusion, such as infection, cancer, or heart failure.
Needle Removal and Dressing
Once the necessary fluid or air has been removed, the needle is withdrawn, and a sterile dressing is applied to the insertion site. Pressure may be applied to prevent bleeding.
Post-Procedure Observation
After thoracentesis, you’ll be monitored for a short period to ensure there are no immediate complications or adverse reactions. Most patients can resume normal activities shortly after the procedure.
Risks and Complications
While thoracentesis is generally considered a safe procedure when performed by skilled healthcare professionals, it’s essential to be aware of potential risks and complications:
Bleeding:
There is a slight risk of bleeding at the needle insertion site. Healthcare providers take precautions to minimize this risk, especially if you are on blood-thinning medications.
Infection:
Although sterile techniques are used, there’s a minimal risk of infection at the puncture site. Inform your healthcare provider if you notice any signs of infection, such as redness, swelling, or increased pain.
Pneumothorax:
In rare cases, thoracentesis may lead to a pneumothorax, where air enters the pleural space, potentially causing lung collapse. Healthcare providers monitor for this complication and take immediate action if necessary.
Discomfort:
Some discomfort is expected during and after the procedure, but it’s typically manageable with over-the-counter pain relievers.
Nerve Injury:
There is a remote risk of injuring nearby nerves during the procedure, which could lead to numbness or weakness in the chest or upper abdomen.
Allergic Reaction:
While rare, allergic reactions to local anesthesia or other medications used during thoracentesis can occur. Be sure to disclose any known allergies to your healthcare provider.
Recovery and Aftercare
Recovery following thoracentesis is generally straightforward:
Observation:
You may be monitored for a short period after the procedure to check for any immediate complications.
Resuming Normal Activities:
Most patients can resume their normal activities within a few hours to a day. However, strenuous activities may be limited for a short time.
Pain Management:
Over-the-counter pain relievers can help manage any discomfort or mild pain at the insertion site.
Follow-Up:
Depending on the reason for the procedure, your healthcare provider may schedule follow-up appointments to discuss test results and ongoing care.
Benefits and Outcomes
Thoracentesis is a valuable medical procedure with several benefits and positive outcomes:
Symptom Relief:
For individuals experiencing symptoms like shortness of breath or chest pain due to pleural effusion or pneumothorax, thoracentesis can provide rapid relief, improving their quality of life.
Accurate Diagnosis:
The procedure allows healthcare providers to collect pleural fluid or air samples for analysis, aiding in the diagnosis of underlying medical conditions, such as infections, cancer, or heart failure.
Treatment Facilitation:
Thoracentesis can serve as both a diagnostic and therapeutic tool. It not only identifies the problem but also helps alleviate it by removing excess fluid or air.
Monitoring Progress:
In cases where patients are undergoing treatment for certain conditions, such as cancer, thoracentesis may be performed periodically to monitor progress and adjust treatment plans accordingly.
Improved Lung Function:
By relieving pressure on the lungs caused by pleural effusion or pneumothorax, thoracentesis can enhance lung function, making it easier to breathe.
FAQs related to thoracentesis along with their answers:
Q1: What is thoracentesis?
A1: Thoracentesis is a medical procedure used to remove excess fluid or air from the pleural space, which is the area between the lung and the chest wall.
Q2: Why is thoracentesis performed?
A2: Thoracentesis is performed for both diagnostic and therapeutic purposes. It helps identify the cause of pleural effusion (fluid buildup) and provides relief for symptoms like shortness of breath and chest pain.
Q3: Is thoracentesis a painful procedure?
A3: While some discomfort may be experienced during the procedure, local anesthesia is typically used to minimize pain, making it tolerable for most patients.
Q4: How long does a thoracentesis procedure take?
A4: The procedure itself usually takes about 15 to 30 minutes, although the total time spent at the medical facility may be longer due to preparation and recovery.
Q5: Are there any risks associated with thoracentesis?
A5: Yes, there are potential risks, including bleeding, infection, pneumothorax (lung collapse), and nerve injury. Your healthcare provider will discuss these risks with you before the procedure.
Q6: What happens to the fluid or air removed during thoracentesis?
A6: The fluid or air removed during thoracentesis may be sent to a laboratory for analysis. This analysis helps determine its composition and underlying cause, aiding in diagnosis and treatment planning.
Q7: How should I prepare for thoracentesis?
A7: Preparation typically involves a medical evaluation, informed consent, fasting, and temporarily discontinuing certain medications. Follow your healthcare provider’s specific instructions.
Q8: What is the recovery process like after thoracentesis?
A8: Recovery is generally straightforward. Patients are monitored briefly after the procedure and can usually resume normal activities within a few hours to a day. Pain can be managed with over-the-counter medications.
Q9: Can thoracentesis be used to treat lung cancer?
A9: Thoracentesis is primarily a diagnostic procedure, but it can provide relief for symptoms related to lung cancer, such as pleural effusion. Treatment for lung cancer depends on various factors and may include other interventions.
Q10: Is thoracentesis safe for pregnant individuals?
A10: The safety of thoracentesis during pregnancy depends on specific circumstances and should be discussed with a healthcare provider. The risks and benefits will be carefully considered to make an informed decision.
Conclusion
In this comprehensive guide, we’ve explored the thoracentesis procedure, from understanding its importance and indications to detailed insights into its steps, risks, and recovery. By demystifying thoracentesis, we hope to empower you with knowledge and alleviate any concerns you may have about this essential medical procedure.